Bij de ontwikkeling van de richtlijn is rekening gehouden met het patiënten perspectief. Edwin Bos, ouder, heeft een actieve bijdrage geleverd aan de werkgroep.
Daarnaast zijn er twee focusgroepen uitgevoerd. Een focusgroep met ouders en een focusgroep met jongeren. In de rapportage van de praktijktest is een uitgebreid verslag van deze focusgroepen te vinden.[167]
8.4 Cliënten participatie
JGZ-richtlijn Gezonde slaap en slaapproblemen bij kinderen
JGZ-richtlijn Gezonde slaap en slaapproblemen bij kinderen
Let op: deze richtlijn is momenteel in herziening.
Dit betekent niet dat de inhoud van deze richtlijn incorrect is. Tot de herziening blijft de richtlijn leidend voor de praktijk. Wel bestaat er een kans dat een deel van de informatie verouderd is.
Heb je feedback over deze JGZ-richtlijn? Stuur jouw feedback naar onze servicedesk. Zoek het tekstgedeelte waarbij je suggesties voor verbetering hebt. Via de knop ‘Geef jouw feedback’ kun je voor deze JGZ-richtlijn en het specifieke hoofdstuk jouw suggesties doorgeven.
Richtlijn inhoudsopgave
1 Inleiding Ga naar pagina over 1 Inleiding
2 Definities en achtergrondinformatie Ga naar pagina over 2 Definities en achtergrondinformatie
3 Risico- en beschermende factoren Ga naar pagina over 3 Risico- en beschermende factoren
4 Preventie Ga naar pagina over 4 Preventie
5 Signaleren, diagnostiek en verwijzen Ga naar pagina over 5 Signaleren, diagnostiek en verwijzen
6 Begeleiden en behandelen Ga naar pagina over 6 Begeleiden en behandelen
7 Samenwerken en doorverwijzen Ga naar pagina over 7 Samenwerken en doorverwijzen
8 Totstandkoming richtlijn Ga naar pagina over 8 Totstandkoming richtlijn
9 Verantwoording Ga naar pagina over 9 Verantwoording
1 Inleiding Ga naar pagina over 1 Inleiding
2 Definities en achtergrondinformatie Ga naar pagina over 2 Definities en achtergrondinformatie
3 Risico- en beschermende factoren Ga naar pagina over 3 Risico- en beschermende factoren
4 Preventie Ga naar pagina over 4 Preventie
5 Signaleren, diagnostiek en verwijzen Ga naar pagina over 5 Signaleren, diagnostiek en verwijzen
6 Begeleiden en behandelen Ga naar pagina over 6 Begeleiden en behandelen
7 Samenwerken en doorverwijzen Ga naar pagina over 7 Samenwerken en doorverwijzen
8 Totstandkoming richtlijn Ga naar pagina over 8 Totstandkoming richtlijn
9 Verantwoording Ga naar pagina over 9 Verantwoording
Heb je suggesties voor verbetering van deze JGZ-richtlijn?
Geef jouw feedbackSamenvattingskaart richtlijn Gezonde slaap en slaapproblemen
PP-presentatie voor scholing Gezonde slaap en slaapproblemen
Randvoorwaardelijke implicaties richtlijn Gezonde slaap en slaapproblemen
Rapportage praktijktest richtlijn Gezonde slaap en slaapproblemen
Indicatoren richtlijn Gezonde slaap en slaapproblemen
Implementatiebijeenkomst Gezonde slaap: vraag en antwoord
Slaaptips om te verspreiden via Social Media
Bijlage 1a Uitgebreide anamnese bij slaapproblemen van kinderen en jongeren
Bijlage 1b. Uitgebreide anamnese bij slaapproblemen van oudere kinderen en pubers
Bijlage 2a Slaaphygiëne Vragenlijst Adolescenten (ASHQ)
Bijlage 2b Chronisch Slaaptekort Vragenlijst kinderen en adolescenten (CSRQ)
Bijlage 3a Slaapdagboek voor kind-jongere 6-18 jaar
Bijlage 3b Slaapdagboekje kinderen 6 maanden tot 4 jaar
Bijlage 6 Slaaptips voor pubers en adolescenten
[1] Paruthi S, Brooks LJ, D'Ambrosio C, Hall WA, Kotagal S, Lloyd RM, Malow BA, Maski K, Nichols C, Quan SF, Rosen CL, Troester MM, Wise MS. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2016;12(6):785-6
http://dx.doi.org/10.5664/jcsm.5866 https://pubmed.ncbi.nlm.nih.gov/27250809[2] Boer F. Slaapproblemen bij kinderen: Kinderpsychologie in de praktijk Lannoo-Meulenhoff Belgium 2013
[3] Galland BC, Taylor BJ, Elder DE, Herbison P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep medicine reviews 2012;16(3):213-22
http://dx.doi.org/10.1016/j.smrv.2011.06.001 https://pubmed.ncbi.nlm.nih.gov/21784676[4] Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 2003;111(2):302-7
https://pubmed.ncbi.nlm.nih.gov/12563055[5] Meijer AM, van den Wittenboer GLH. Contribution of infants' sleep and crying to marital relationship of first-time parent couples in the 1st year after childbirth. Journal of family psychology : JFP : journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2007;21(1):49-57
https://pubmed.ncbi.nlm.nih.gov/17371109[6] Henderson JMT, France KG, Owens JL, Blampied NM. Sleeping through the night: the consolidation of self-regulated sleep across the first year of life. Pediatrics 2010;126(5):e1081-7
http://dx.doi.org/10.1542/peds.2010-0976 https://pubmed.ncbi.nlm.nih.gov/20974775[7] van Litsenburg RRL, Waumans RC, van den Berg G, Gemke RJBJ. Sleep habits and sleep disturbances in Dutch children: a population-based study. European journal of pediatrics 2010;169(8):1009-15
http://dx.doi.org/10.1007/s00431-010-1169-8 https://pubmed.ncbi.nlm.nih.gov/20191392[8] van der Heijden KB, de Sonneville LMJ, Swaab H. Association of eveningness with problem behavior in children: a mediating role of impaired sleep. Chronobiology international 2013;30(7):919-29
http://dx.doi.org/10.3109/07420528.2013.790041 https://pubmed.ncbi.nlm.nih.gov/23802509[9] Owens JA, Belon K, Moss P. Impact of delaying school start time on adolescent sleep, mood, and behavior. Archives of pediatrics & adolescent medicine 2010;164(7):608-14
http://dx.doi.org/10.1001/archpediatrics.2010.96 https://pubmed.ncbi.nlm.nih.gov/20603459[10] Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep medicine 2011;12(2):110-8
http://dx.doi.org/10.1016/j.sleep.2010.11.008 https://pubmed.ncbi.nlm.nih.gov/21257344[11] American Academy of Sleep Medicine. International classification of sleep disorders—third edition (ICSD-3) AASM Resource Library [online] 2014
[12] American Psychiatric Association. Diagnostic and statistical manual of mental disorders 5th ed. 2013
[13] American Academy of Sleep Medicine. International classification of sleep disorders. 2nd ed. Westchester, IL 2005
[14] Jenni OG, Fuhrer HZ, Iglowstein I, Molinari L, Largo RH. A longitudinal study of bed sharing and sleep problems among Swiss children in the first 10 years of life. Pediatrics 2005;115(1 Suppl):233-40
https://pubmed.ncbi.nlm.nih.gov/15866857[15] Byars KC, Yolton K, Rausch J, Lanphear B, Beebe DW. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics 2012;129(2):e276-84
http://dx.doi.org/10.1542/peds.2011-0372 https://pubmed.ncbi.nlm.nih.gov/22218837[16] Meltzer LJ, Plaufcan MR, Thomas JH, Mindell JA. Sleep problems and sleep disorders in pediatric primary care: treatment recommendations, persistence, and health care utilization. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2014;10(4):421-6
http://dx.doi.org/10.5664/jcsm.3620 https://pubmed.ncbi.nlm.nih.gov/24733988[17] van Sleuwen BE, Vlasblom E, L'Hoir MP. Eindverslag laagdrempelige verpleegkundige interventiemethoden in de jeugdgezondheidszorg bij slaapproblemen van jonge kinderen. ZonMW 2013
http://www.zonmw.nl/nl/projecten/project-detail/laagdrempelige-verpleegkundige-interventiemethoden-in-de-jeugdgezondheidszorg-bij-slaapproblemen-van/voortgang/[18] Linden M, Suijlekom-Smit L, Schellevis FG, Wouden J. Tweede nationale studie naar ziekten en verrichtingen in de huisartspraktijk. het kind in de huisartspraktijk. Utrecht: Nivel 2005
[19] Yperen T, Stam PT. Opvoeden versterken. Den Haag: VNG 2010
[20] Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A, . Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep 2006;29(10):1263-76
https://pubmed.ncbi.nlm.nih.gov/17068979[21] Ednick M, Cohen AP, McPhail GL, Beebe D, Simakajornboon N, Amin RS. A review of the effects of sleep during the first year of life on cognitive, psychomotor, and temperament development. Sleep 2009;32(11):1449-58
https://pubmed.ncbi.nlm.nih.gov/19928384[22] Hemmi MH, Wolke D, Schneider S. Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioural outcomes in childhood: a meta-analysis. Archives of disease in childhood 2011;96(7):622-9
http://dx.doi.org/10.1136/adc.2010.191312 https://pubmed.ncbi.nlm.nih.gov/21508059[23] Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK. Acute sleep restriction effects on emotion responses in 30- to 36-month-old children. Journal of sleep research 2012;21(3):235-46
http://dx.doi.org/10.1111/j.1365-2869.2011.00962.x https://pubmed.ncbi.nlm.nih.gov/21988087[24] Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep medicine reviews 2010;14(3):179-89
http://dx.doi.org/10.1016/j.smrv.2009.10.004 https://pubmed.ncbi.nlm.nih.gov/20093054[25] Koulouglioti C, Cole R, Kitzman H. Inadequate sleep and unintentional injuries in young children. Public health nursing (Boston, Mass.) 2008;25(2):106-14
http://dx.doi.org/10.1111/j.1525-1446.2008.00687.x https://pubmed.ncbi.nlm.nih.gov/18294179[26] Gregory AM, Van der Ende J, Willis TA, Verhulst FC. Parent-reported sleep problems during development and self-reported anxiety/depression, attention problems, and aggressive behavior later in life. Archives of pediatrics & adolescent medicine 2008;162(4):330-5
http://dx.doi.org/10.1001/archpedi.162.4.330 https://pubmed.ncbi.nlm.nih.gov/18391141[27] Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van Lenthe FJ, Brug J. Early-life determinants of overweight and obesity: a review of systematic reviews. Obesity reviews : an official journal of the International Association for the Study of Obesity 2010;11(10):695-708
http://dx.doi.org/10.1111/j.1467-789X.2010.00735.x https://pubmed.ncbi.nlm.nih.gov/20331509[28] Astill RG, Van der Heijden KB, Van Ijzendoorn MH, Van Someren EJW. Sleep, cognition, and behavioral problems in school-age children: a century of research meta-analyzed. Psychological bulletin 2012;138(6):1109-38
http://dx.doi.org/10.1037/a0028204 https://pubmed.ncbi.nlm.nih.gov/22545685[29] Owens J, Gruber R, Brown T, Corkum P, Cortese S, O'Brien L, Stein M, Weiss M. Future research directions in sleep and ADHD: report of a consensus working group. Journal of attention disorders 2013;17(7):550-64
http://dx.doi.org/10.1177/1087054712457992 https://pubmed.ncbi.nlm.nih.gov/22982880[30] Kheirandish L, Gozal D. Neurocognitive dysfunction in children with sleep disorders. Developmental science 2006;9(4):388-99
https://pubmed.ncbi.nlm.nih.gov/16764612[31] Nielsen LS, Danielsen KV, Sørensen TIA. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obesity reviews : an official journal of the International Association for the Study of Obesity 2011;12(2):78-92
http://dx.doi.org/10.1111/j.1467-789X.2010.00724.x https://pubmed.ncbi.nlm.nih.gov/20345429[32] Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep medicine reviews 2014;18(1):75-87
http://dx.doi.org/10.1016/j.smrv.2013.03.005 https://pubmed.ncbi.nlm.nih.gov/23806891[33] Moore M, Meltzer LJ. The sleepy adolescent: causes and consequences of sleepiness in teens. Paediatric respiratory reviews 2008;9(2):114-20; quiz 120-1
http://dx.doi.org/10.1016/j.prrv.2008.01.001 https://pubmed.ncbi.nlm.nih.gov/18513671[34] Vallido T, Peters K, O'Brien L, Jackson D. Sleep in adolescence: a review of issues for nursing practice. Journal of clinical nursing 2009;18(13):1819-26
http://dx.doi.org/10.1111/j.1365-2702.2009.02812.x https://pubmed.ncbi.nlm.nih.gov/19638045[35] de Bruin EJ, van Run C, Staaks J, Meijer AM. Effects of sleep manipulation on cognitive functioning of adolescents: A systematic review. Sleep medicine reviews 2017;32():45-57
http://dx.doi.org/10.1016/j.smrv.2016.02.006 https://pubmed.ncbi.nlm.nih.gov/27039223[36] Rutters F, Gerver WJ, Nieuwenhuizen AG, Verhoef SPM, Westerterp-Plantenga MS. Sleep duration and body-weight development during puberty in a Dutch children cohort. International journal of obesity (2005) 2010;34(10):1508-14
http://dx.doi.org/10.1038/ijo.2010.161 https://pubmed.ncbi.nlm.nih.gov/20714331[37] Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Association of short and long sleep durations with insulin sensitivity in adolescents. The Journal of pediatrics 2011;158(4):617-23
http://dx.doi.org/10.1016/j.jpeds.2010.09.080 https://pubmed.ncbi.nlm.nih.gov/21146189[38] Faraut B, Boudjeltia KZ, Vanhamme L, Kerkhofs M. Immune, inflammatory and cardiovascular consequences of sleep restriction and recovery. Sleep medicine reviews 2012;16(2):137-49
http://dx.doi.org/10.1016/j.smrv.2011.05.001 https://pubmed.ncbi.nlm.nih.gov/21835655[39] Orzech KM, Acebo C, Seifer R, Barker D, Carskadon MA. Sleep patterns are associated with common illness in adolescents. Journal of sleep research 2014;23(2):133-42
http://dx.doi.org/10.1111/jsr.12096 https://pubmed.ncbi.nlm.nih.gov/24134661[40] Mindell JA, Telofski LS, Wiegand B, Kurtz ES. A nightly bedtime routine: impact on sleep in young children and maternal mood. Sleep 2009;32(5):599-606
https://pubmed.ncbi.nlm.nih.gov/19480226[41] Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep medicine reviews 2010;14(2):89-96
http://dx.doi.org/10.1016/j.smrv.2009.05.003 https://pubmed.ncbi.nlm.nih.gov/19631566[42] Martin J, Hiscock H, Hardy P, Davey B, Wake M. Adverse associations of infant and child sleep problems and parent health: an Australian population study. Pediatrics 2007;119(5):947-55
https://pubmed.ncbi.nlm.nih.gov/17473096[43] Hunter LP, Rychnovsky JD, Yount SM. A selective review of maternal sleep characteristics in the postpartum period. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN 2009;38(1):60-8
http://dx.doi.org/10.1111/j.1552-6909.2008.00309.x https://pubmed.ncbi.nlm.nih.gov/19208049[44] Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep medicine 2009;10(7):771-9
http://dx.doi.org/10.1016/j.sleep.2008.07.016 https://pubmed.ncbi.nlm.nih.gov/19285450[45] Semple A. What influences baby-sleeping behaviour at night (1)? The practising midwife 2010;13(9):17-20
https://pubmed.ncbi.nlm.nih.gov/21138130[46] Malone SK. Early to bed, early to rise?: an exploration of adolescent sleep hygiene practices. The Journal of school nursing : the official publication of the National Association of School Nurses 2011;27(5):348-54
http://dx.doi.org/10.1177/1059840511410434 https://pubmed.ncbi.nlm.nih.gov/21606219[47] de Bruin EJ, van Kampen RKA, van Kooten T, Meijer AM. Psychometric properties and clinical relevance of the adolescent sleep hygiene scale in Dutch adolescents. Sleep medicine 2014;15(7):789-97
http://dx.doi.org/10.1016/j.sleep.2014.03.015 https://pubmed.ncbi.nlm.nih.gov/24891082[48] Galbally M, Lewis AJ, McEgan K, Scalzo K, Islam FA. Breastfeeding and infant sleep patterns: an Australian population study. Journal of paediatrics and child health 2013;49(2):E147-52
http://dx.doi.org/10.1111/jpc.12089 https://pubmed.ncbi.nlm.nih.gov/23331519[49] Ramamurthy MB, Sekartini R, Ruangdaraganon N, Huynh DHT, Sadeh A, Mindell JA. Effect of current breastfeeding on sleep patterns in infants from Asia-Pacific region. Journal of paediatrics and child health 2012;48(8):669-74
http://dx.doi.org/10.1111/j.1440-1754.2012.02453.x https://pubmed.ncbi.nlm.nih.gov/22616943[50] Rosen LA. Infant sleep and feeding. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN 2008;37(6):706-14
http://dx.doi.org/10.1111/j.1552-6909.2008.00299.x https://pubmed.ncbi.nlm.nih.gov/19012721[51] Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breastfeeding medicine : the official journal of the Academy of Breastfeeding Medicine 2015;10(5):246-52
http://dx.doi.org/10.1089/bfm.2014.0153 https://pubmed.ncbi.nlm.nih.gov/25973527[52] Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep medicine 2010;11(8):735-42
http://dx.doi.org/10.1016/j.sleep.2010.02.006 https://pubmed.ncbi.nlm.nih.gov/20673649[53] Vijakkhana N, Wilaisakditipakorn T, Ruedeekhajorn K, Pruksananonda C, Chonchaiya W. Evening media exposure reduces night-time sleep. Acta paediatrica (Oslo, Norway : 1992) 2015;104(3):306-12
http://dx.doi.org/10.1111/apa.12904 https://pubmed.ncbi.nlm.nih.gov/25521612[54] Falbe J, Davison KK, Franckle RL, Ganter C, Gortmaker SL, Smith L, Land T, Taveras EM. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 2015;135(2):e367-75
http://dx.doi.org/10.1542/peds.2014-2306 https://pubmed.ncbi.nlm.nih.gov/25560435[55] Owens JA, Mindell J, Baylor A. Effect of energy drink and caffeinated beverage consumption on sleep, mood, and performance in children and adolescents. Nutrition reviews 2014;72 Suppl 1():65-71
http://dx.doi.org/10.1111/nure.12150 https://pubmed.ncbi.nlm.nih.gov/25293545[56] Mathers M, Toumbourou JW, Catalano RF, Williams J, Patton GC. Consequences of youth tobacco use: a review of prospective behavioural studies. Addiction (Abingdon, England) 2006;101(7):948-58
https://pubmed.ncbi.nlm.nih.gov/16771887[57] Patten CA, Choi WS, Gillin JC, Pierce JP. Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics 2000;106(2):E23
https://pubmed.ncbi.nlm.nih.gov/10920179[58] Pasch KE, Latimer LA, Cance JD, Moe SG, Lytle LA. Longitudinal bi-directional relationships between sleep and youth substance use. Journal of youth and adolescence 2012;41(9):1184-96
http://dx.doi.org/10.1007/s10964-012-9784-5 https://pubmed.ncbi.nlm.nih.gov/22752878[59] O'Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behavioral sleep medicine 2005;3(3):113-33
https://pubmed.ncbi.nlm.nih.gov/15984914[60] Treyster Z, Gitterman B. Second hand smoke exposure in children: environmental factors, physiological effects, and interventions within pediatrics. Reviews on environmental health 2011;26(3):187-95
https://pubmed.ncbi.nlm.nih.gov/22206195[61] Wong MM, Robertson GC, Dyson RB. Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcoholism, clinical and experimental research 2015;39(2):355-62
http://dx.doi.org/10.1111/acer.12618 https://pubmed.ncbi.nlm.nih.gov/25598438[62] Roberts RE, Roberts CR, Duong HT. Sleepless in adolescence: prospective data on sleep deprivation, health and functioning. Journal of adolescence 2009;32(5):1045-57
http://dx.doi.org/10.1016/j.adolescence.2009.03.007 https://pubmed.ncbi.nlm.nih.gov/19361854[63] Wahlstrom K, Dretzke B, Gordon M, Peterson K, Edwards K, Gdula J. Examining the Impact of Later School Start Times on the Health and Academic Performance of High School Students: A Multi-Site Study Center for Applied Research and Educational Improvement. St Paul, MN: University of Minnesota. 2014
[64] Danner F, Phillips B. Adolescent sleep, school start times, and teen motor vehicle crashes. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2008;4(6):533-5
https://pubmed.ncbi.nlm.nih.gov/19110880[65] Labree LJWW, van de Mheen HD, Rutten FFHF, Rodenburg GG, Koopmans GTG, Foets MM. Sleep duration differences between children of migrant and native origins. Zeitschrift fur Gesundheitswissenschaften = Journal of public health 2015;23(3):149-156
https://pubmed.ncbi.nlm.nih.gov/26000233[66] Knutson KL. Sociodemographic and cultural determinants of sleep deficiency: implications for cardiometabolic disease risk. Social science & medicine (1982) 2013;79():7-15
http://dx.doi.org/10.1016/j.socscimed.2012.05.002 https://pubmed.ncbi.nlm.nih.gov/22682665[67] Mindell JA, Sadeh A, Kohyama J, How TH. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep medicine 2010;11(4):393-9
http://dx.doi.org/10.1016/j.sleep.2009.11.011 https://pubmed.ncbi.nlm.nih.gov/20223706[68] Olds T, Blunden S, Petkov J, Forchino F. The relationships between sex, age, geography and time in bed in adolescents: a meta-analysis of data from 23 countries. Sleep medicine reviews 2010;14(6):371-8
http://dx.doi.org/10.1016/j.smrv.2009.12.002 https://pubmed.ncbi.nlm.nih.gov/20207558[69] Schredl M, Reinhard I. Gender differences in nightmare frequency: a meta-analysis. Sleep medicine reviews 2011;15(2):115-21
http://dx.doi.org/10.1016/j.smrv.2010.06.002 https://pubmed.ncbi.nlm.nih.gov/20817509[70] Meijer AM, Habekothé HT, Van Den Wittenboer GL. Time in bed, quality of sleep and school functioning of children. Journal of sleep research 2000;9(2):145-53
https://pubmed.ncbi.nlm.nih.gov/10849241[71] Konofal E, Lecendreux M, Cortese S. Sleep and ADHD. Sleep medicine 2010;11(7):652-8
http://dx.doi.org/10.1016/j.sleep.2010.02.012 https://pubmed.ncbi.nlm.nih.gov/20620109[72] Sadeh A, Pergamin L, Bar-Haim Y. Sleep in children with attention-deficit hyperactivity disorder: a meta-analysis of polysomnographic studies. Sleep medicine reviews 2006;10(6):381-98
https://pubmed.ncbi.nlm.nih.gov/16846743[73] Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. Journal of the American Academy of Child and Adolescent Psychiatry 2009;48(9):894-908
http://dx.doi.org/10.1097/CHI.0b013e3181ac09c9 https://pubmed.ncbi.nlm.nih.gov/19625983[74] Bullock GL, Schall U. Dyssomnia in children diagnosed with attention deficit hyperactivity disorder: a critical review. The Australian and New Zealand journal of psychiatry 2005;39(5):373-7
https://pubmed.ncbi.nlm.nih.gov/15860025[75] Ivanenko A, Johnson K. Sleep disturbances in children with psychiatric disorders. Seminars in pediatric neurology 2008;15(2):70-8
http://dx.doi.org/10.1016/j.spen.2008.03.008 https://pubmed.ncbi.nlm.nih.gov/18555193[76] Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep medicine reviews 2012;16(3):231-41
http://dx.doi.org/10.1016/j.smrv.2011.05.005 https://pubmed.ncbi.nlm.nih.gov/21784678[77] Liu J, Zhang A, Li L. Sleep duration and overweight/obesity in children: review and implications for pediatric nursing. Journal for specialists in pediatric nursing : JSPN 2012;17(3):193-204
http://dx.doi.org/10.1111/j.1744-6155.2012.00332.x https://pubmed.ncbi.nlm.nih.gov/22734873[78] Kuhl ES, Clifford LM, Stark LJ. Obesity in preschoolers: behavioral correlates and directions for treatment. Obesity (Silver Spring, Md.) 2012;20(1):3-29
http://dx.doi.org/10.1038/oby.2011.201 https://pubmed.ncbi.nlm.nih.gov/21760634[79] Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring, Md.) 2008;16(2):265-74
http://dx.doi.org/10.1038/oby.2007.63 https://pubmed.ncbi.nlm.nih.gov/18239632[80] Cappuccio FP, Taggart FM, Kandala N-B, Currie A, Peile ED, Stranges S, Miller MA. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008;31(5):619-26
https://pubmed.ncbi.nlm.nih.gov/18517032[81] Hollway JA, Aman MG. Sleep correlates of pervasive developmental disorders: a review of the literature. Research in developmental disabilities 2011;32(5):1399-421
http://dx.doi.org/10.1016/j.ridd.2011.04.001 https://pubmed.ncbi.nlm.nih.gov/21570809[82] Valrie CR, Bromberg MH, Palermo T, Schanberg LE. A systematic review of sleep in pediatric pain populations. Journal of developmental and behavioral pediatrics : JDBP 2013;34(2):120-8
http://dx.doi.org/10.1097/DBP.0b013e31827d5848 https://pubmed.ncbi.nlm.nih.gov/23369958[83] Tietze A-L, Blankenburg M, Hechler T, Michel E, Koh M, Schlüter B, Zernikow B. Sleep disturbances in children with multiple disabilities. Sleep medicine reviews 2012;16(2):117-27
http://dx.doi.org/10.1016/j.smrv.2011.03.006 https://pubmed.ncbi.nlm.nih.gov/21620745[84] Yilmaz E, Sedky K, Bennett DS. The relationship between depressive symptoms and obstructive sleep apnea in pediatric populations: a meta-analysis. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2013;9(11):1213-20
http://dx.doi.org/10.5664/jcsm.3178 https://pubmed.ncbi.nlm.nih.gov/24235907[85] Kowatch RA, Youngstrom EA, Danielyan A, Findling RL. Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar disorders 2005;7(6):483-96
https://pubmed.ncbi.nlm.nih.gov/16403174[86] Cairns KE, Yap MBH, Pilkington PD, Jorm AF. Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. Journal of affective disorders 2014;169():61-75
http://dx.doi.org/10.1016/j.jad.2014.08.006 https://pubmed.ncbi.nlm.nih.gov/25154536[87] Augustinavicius JLS, Zanjani A, Zakzanis KK, Shapiro CM. Polysomnographic features of early-onset depression: a meta-analysis. Journal of affective disorders 2014;158():11-8
http://dx.doi.org/10.1016/j.jad.2013.12.009 https://pubmed.ncbi.nlm.nih.gov/24655760[88] Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. The Journal of clinical psychiatry 2012;73(9):e1160-7
http://dx.doi.org/10.4088/JCP.11r07586 https://pubmed.ncbi.nlm.nih.gov/23059158[89] Churchill SS, Kieckhefer GM, Bjornson KF, Herting JR. Relationship between sleep disturbance and functional outcomes in daily life habits of children with Down syndrome. Sleep 2015;38(1):61-71
http://dx.doi.org/10.5665/sleep.4326 https://pubmed.ncbi.nlm.nih.gov/25325444[90] van Golde EGA, Gutter T, de Weerd AW. Sleep disturbances in people with epilepsy; prevalence, impact and treatment. Sleep medicine reviews 2011;15(6):357-68
http://dx.doi.org/10.1016/j.smrv.2011.01.002 https://pubmed.ncbi.nlm.nih.gov/21439869[91] Charuvastra A, Cloitre M. Safe enough to sleep: sleep disruptions associated with trauma, posttraumatic stress, and anxiety in children and adolescents. Child and adolescent psychiatric clinics of North America 2009;18(4):877-91
http://dx.doi.org/10.1016/j.chc.2009.04.002 https://pubmed.ncbi.nlm.nih.gov/19836694[92] Camfferman D, Kennedy JD, Gold M, Martin AJ, Winwood P, Lushington K. Eczema, sleep, and behavior in children. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2010;6(6):581-8
https://pubmed.ncbi.nlm.nih.gov/21206547[93] Camfferman D, Kennedy JD, Gold M, Simpson C, Lushington K. Sleep and neurocognitive functioning in children with eczema. International journal of psychophysiology : official journal of the International Organization of Psychophysiology 2013;89(2):265-72
http://dx.doi.org/10.1016/j.ijpsycho.2013.01.006 https://pubmed.ncbi.nlm.nih.gov/23353660[94] Ryborg CT, Søndergaard J, Lous J, Munck A, Larsen PV, Thomsen JL. Associations between symptoms, clinical findings and the short-term prognosis among children with otitis media: a cohort study. International journal of pediatric otorhinolaryngology 2013;77(2):210-5
http://dx.doi.org/10.1016/j.ijporl.2012.10.023 https://pubmed.ncbi.nlm.nih.gov/23200872[95] McCormick DP, Jennings K, Ede LC, Alvarez-Fernandez P, Patel J, Chonmaitree T. Use of symptoms and risk factors to predict acute otitis media in infants. International journal of pediatric otorhinolaryngology 2016;81():55-9
http://dx.doi.org/10.1016/j.ijporl.2015.12.002 https://pubmed.ncbi.nlm.nih.gov/26810291[96] Laine MK, Tähtinen PA, Ruuskanen O, Huovinen P, Ruohola A. Symptoms or symptom-based scores cannot predict acute otitis media at otitis-prone age. Pediatrics 2010;125(5):e1154-61
http://dx.doi.org/10.1542/peds.2009-2689 https://pubmed.ncbi.nlm.nih.gov/20368317[97] Üçer O, Gümüş B. Quantifying subjective assessment of sleep quality, quality of life and depressed mood in children with enuresis. World journal of urology 2014;32(1):239-43
http://dx.doi.org/10.1007/s00345-013-1193-1 https://pubmed.ncbi.nlm.nih.gov/24150187[98] Azevedo Soster L, Alves R, Fagundes SN, Koch VHK, Bruni O. Sleep disturbances associated with sleep enuresis: A questionnaire study. European journal of paediatric neurology : EJPN : official journal of the European Paediatric Neurology Society 2016;20(2):282-285
http://dx.doi.org/10.1016/j.ejpn.2015.11.014 https://pubmed.ncbi.nlm.nih.gov/26732069[99] Costigan SA, Barnett L, Plotnikoff RC, Lubans DR. The health indicators associated with screen-based sedentary behavior among adolescent girls: a systematic review. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 2013;52(4):382-92
http://dx.doi.org/10.1016/j.jadohealth.2012.07.018 https://pubmed.ncbi.nlm.nih.gov/23299000[100] Owens J, , . Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics 2014;134(3):e921-32
http://dx.doi.org/10.1542/peds.2014-1696 https://pubmed.ncbi.nlm.nih.gov/25157012[101] Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep medicine reviews 2015;21():50-8
http://dx.doi.org/10.1016/j.smrv.2014.07.007 https://pubmed.ncbi.nlm.nih.gov/25193149[102] Kirby MF, Maggi S, D'Angiulli A. School Start Times and the Sleep–Wake Cycle of Adolescents Educational Researcher 2011;40(2):56
https://www.researchgate.net/publication/258134857_School_Start_Times_and_the_Sleep-Wake_Cycle_of_Adolescents[103] Kelley P, Lockley SW, Foster RG, Kelley J. Synchronizing education to adolescent biology: 'Let teens sleep, start school later' Learning Media and Technology 2014;40(2):1
https://www.researchgate.net/publication/271991912_Synchronizing_education_to_adolescent_biology_'let_teens_sleep_start_school_later'[104] Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children. Sleep 2005;28(12):1568-77
https://pubmed.ncbi.nlm.nih.gov/16408417[105] Cornelius LJ. Health habits of school-age children. Journal of health care for the poor and underserved 1991;2(3):374-95
https://pubmed.ncbi.nlm.nih.gov/1772949[106] McLaughlin Crabtree V, Beal Korhonen J, Montgomery-Downs HE, Faye Jones V, O'Brien LM, Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep medicine 2005;6(4):319-24
https://pubmed.ncbi.nlm.nih.gov/15978515[107] Marco CA, Wolfson AR, Sparling M, Azuaje A. Family socioeconomic status and sleep patterns of young adolescents. Behavioral sleep medicine 2011;10(1):70-80
http://dx.doi.org/10.1080/15402002.2012.636298 https://pubmed.ncbi.nlm.nih.gov/22250780[108] Guérin N, Reinberg A, Testu F, Boulenguiez S, Mechkouri M, Touitou Y. Role of school schedule, age, and parental socioeconomic status on sleep duration and sleepiness of Parisian children. Chronobiology international 2001;18(6):1005-17
https://pubmed.ncbi.nlm.nih.gov/11777075[109] Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep medicine reviews 2008;12(4):289-98
http://dx.doi.org/10.1016/j.smrv.2008.03.001 https://pubmed.ncbi.nlm.nih.gov/18485764[110] Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring, Md.) 2008;16(3):643-53
http://dx.doi.org/10.1038/oby.2007.118 https://pubmed.ncbi.nlm.nih.gov/18239586[111] L'Hoir MP, Vlasblom E, Boere-Boonekamp MM, van Dommelen P, Schmelt D, Dreiskaemper D, Naul R. Slaap en overgewicht in Europees onderzoek: Gezonde Kinderen in een Gezonde Kindomgeving (GKGK). Tijdschrift Jeugdgezondheidszorg 2012;44(6):102
[112] Douglas PS, Hill PS. Behavioral sleep interventions in the first six months of life do not improve outcomes for mothers or infants: a systematic review. Journal of developmental and behavioral pediatrics : JDBP 2013;34(7):497-507
http://dx.doi.org/10.1097/DBP.0b013e31829cafa6 https://pubmed.ncbi.nlm.nih.gov/24042081[113] Blunden SL, Chapman J, Rigney GA. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep medicine reviews 2012;16(4):355-70
http://dx.doi.org/10.1016/j.smrv.2011.08.002 https://pubmed.ncbi.nlm.nih.gov/22104441[114] Bryanton J, Beck CT, Montelpare W. Postnatal parental education for optimizing infant general health and parent-infant relationships. The Cochrane database of systematic reviews 2013
http://dx.doi.org/10.1002/14651858.CD004068.pub4 https://pubmed.ncbi.nlm.nih.gov/24284872[115] Bakker-Camu GJW, Nawijn L, van Sleuwen BE, L'Hoir MP. Preventie van slaapproblemen bij jonge kinderen. Review van de effectieve elementen. Tijdschrift Jeugdgezondheidszorg 2011;43(2):26
[116] Crichton GE, Symon B. Behavioral Management of Sleep Problems in Infants Under 6 Months--What Works? Journal of developmental and behavioral pediatrics : JDBP 2016;37(2):164-71
http://dx.doi.org/10.1097/DBP.0000000000000257 https://pubmed.ncbi.nlm.nih.gov/26836644[117] Allen SL, Howlett MD, Coulombe JA, Corkum PV. ABCs of SLEEPING: A review of the evidence behind pediatric sleep practice recommendations. Sleep medicine reviews 2016;29():1-14
http://dx.doi.org/10.1016/j.smrv.2015.08.006 https://pubmed.ncbi.nlm.nih.gov/26551999[118] Bennett C, Underdown A, Barlow J. Massage for promoting mental and physical health in typically developing infants under the age of six months. The Cochrane database of systematic reviews 2013;2013(4):CD005038
http://dx.doi.org/10.1002/14651858.CD005038.pub3 https://pubmed.ncbi.nlm.nih.gov/23633323[119] Underdown A, Barlow J, Stewart-Brown S. Tactile stimulation in physically healthy infants: Results of a systematic review. Journal of Reproductive and Infant Psychology 2010;28(1):11
[120] van der Lely S, Frey S, Garbazza C, Wirz-Justice A, Jenni OG, Steiner R, Wolf S, Cajochen C, Bromundt V, Schmidt C. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 2015;56(1):113-9
http://dx.doi.org/10.1016/j.jadohealth.2014.08.002 https://pubmed.ncbi.nlm.nih.gov/25287985[121] Burkhart K, Phelps JR. Amber lenses to block blue light and improve sleep: a randomized trial. Chronobiology international 2009;26(8):1602-12
http://dx.doi.org/10.3109/07420520903523719 https://pubmed.ncbi.nlm.nih.gov/20030543[122] Chellappa SL, Gordijn MCM, Cajochen C. Can light make us bright? Effects of light on cognition and sleep. Progress in brain research 2011;190():119-33
http://dx.doi.org/10.1016/B978-0-444-53817-8.00007-4 https://pubmed.ncbi.nlm.nih.gov/21531248[123] Spencer JA, Moran DJ, Lee A, Talbert D. White noise and sleep induction. Archives of disease in childhood 1990;65(1):135-7
https://pubmed.ncbi.nlm.nih.gov/2405784[124] Forquer LM, Johnson C. Continuous White Noise to Reduce Resistance Going to Sleep and Night Wakings in Toddlers Child & Family Behavior Therapy 2005;27(2):1
[125] Waumans RC, Terwee CB, Van den Berg G, Knol DL, Van Litsenburg RRL, Gemke RJBJ. Sleep and sleep disturbance in children: Reliability and validity of the Dutch version of the Child Sleep Habits Questionnaire. Sleep 2010;33(6):841-5
https://pubmed.ncbi.nlm.nih.gov/20550026[126] Dewald JF, Short MA, Gradisar M, Oort FJ, Meijer AM. The Chronic Sleep Reduction Questionnaire (CSRQ): a cross-cultural comparison and validation in Dutch and Australian adolescents. Journal of sleep research 2012;21(5):584-94
http://dx.doi.org/10.1111/j.1365-2869.2012.00999.x https://pubmed.ncbi.nlm.nih.gov/22329363[127] Ramdurg S. Kleine-Levin syndrome: Etiology, diagnosis, and treatment. Annals of Indian Academy of Neurology 2010;13(4):241-6
http://dx.doi.org/10.4103/0972-2327.74185 https://pubmed.ncbi.nlm.nih.gov/21264130[128] Simakajornboon N, Kheirandish-Gozal L, Gozal D. Diagnosis and management of restless legs syndrome in children. Sleep medicine reviews 2009;13(2):149-56
http://dx.doi.org/10.1016/j.smrv.2008.12.002 https://pubmed.ncbi.nlm.nih.gov/19186083[129] Meijer AM, Hofman W. Assessment en protocollaire behandeling van slaapproblemen bij kinderen Protocollaire behandelingen voor kinderen met psychische klachten 2014
[130] Morgenthaler TI, Owens J, Alessi C, Boehlecke B, Brown TM, Coleman J, Friedman L, Kapur VK, Lee-Chiong T, Pancer J, Swick TJ, . Practice parameters for behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep 2006;29(10):1277-81
https://pubmed.ncbi.nlm.nih.gov/17068980[131] Brown CA, Kuo M, Phillips L, Berry R, Tan M. Non-pharmacological sleep interventions for youth with chronic health conditions: a critical review of the methodological quality of the evidence. Disability and rehabilitation 2013;35(15):1221-55
http://dx.doi.org/10.3109/09638288.2012.723788 https://pubmed.ncbi.nlm.nih.gov/23050860[132] Escalona A, Field T, Singer-Strunck R, Cullen C, Hartshorn K. Brief report: improvements in the behavior of children with autism following massage therapy. Journal of autism and developmental disorders 2001;31(5):513-6
https://pubmed.ncbi.nlm.nih.gov/11794416[133] Dobson D, Lucassen PLBJ, Miller JJ, Vlieger AM, Prescott P, Lewith G. Manipulative therapies for infantile colic. The Cochrane database of systematic reviews 2012;12():CD004796
http://dx.doi.org/10.1002/14651858.CD004796.pub2 https://pubmed.ncbi.nlm.nih.gov/23235617[134] McRury JM, Zolotor AJ. A randomized, controlled trial of a behavioral intervention to reduce crying among infants. Journal of the American Board of Family Medicine : JABFM 2010;23(3):315-22
http://dx.doi.org/10.3122/jabfm.2010.03.090142 https://pubmed.ncbi.nlm.nih.gov/20453177[135] Quach J, Hiscock H, Ukoumunne OC, Wake M. A brief sleep intervention improves outcomes in the school entry year: a randomized controlled trial. Pediatrics 2011;128(4):692-701
http://dx.doi.org/10.1542/peds.2011-0409 https://pubmed.ncbi.nlm.nih.gov/21890825[136] Sciberras E, Fulton M, Efron D, Oberklaid F, Hiscock H. Managing sleep problems in school aged children with ADHD: a pilot randomised controlled trial. Sleep medicine 2011;12(9):932-5
http://dx.doi.org/10.1016/j.sleep.2011.02.006 https://pubmed.ncbi.nlm.nih.gov/22005602[137] Moore BA, Friman PC, Fruzzetti AE, MacAleese K. Brief report: evaluating the Bedtime Pass Program for child resistance to bedtime--a randomized, controlled trial. Journal of pediatric psychology 2007;32(3):283-7
https://pubmed.ncbi.nlm.nih.gov/16899650[138] Gradisar M, Dohnt H, Gardner G, Paine S, Starkey K, Menne A, Slater A, Wright H, Hudson JL, Weaver E, Trenowden S. A randomized controlled trial of cognitive-behavior therapy plus bright light therapy for adolescent delayed sleep phase disorder. Sleep 2011;34(12):1671-80
http://dx.doi.org/10.5665/sleep.1432 https://pubmed.ncbi.nlm.nih.gov/22131604[139] de Bruin EJ, Bögels SM, Oort FJ, Meijer AM. Efficacy of Cognitive Behavioral Therapy for Insomnia in Adolescents: A Randomized Controlled Trial with Internet Therapy, Group Therapy and A Waiting List Condition. Sleep 2015;38(12):1913-26
http://dx.doi.org/10.5665/sleep.5240 https://pubmed.ncbi.nlm.nih.gov/26158889[140] de Bruin EJ, Oort FJ, Bögels SM, Meijer AM. Efficacy of internet and group-administered cognitive behavioral therapy for insomnia in adolescents: a pilot study. Behavioral sleep medicine 2014;12(3):235-54
http://dx.doi.org/10.1080/15402002.2013.784703 https://pubmed.ncbi.nlm.nih.gov/23767888[141] Bendz LM, Scates AC. Melatonin treatment for insomnia in pediatric patients with attention-deficit/hyperactivity disorder. The Annals of pharmacotherapy 2010;44(1):185-91
http://dx.doi.org/10.1345/aph.1M365 https://pubmed.ncbi.nlm.nih.gov/20028959[142] van Geijlswijk IM, Korzilius HPLM, Smits MG. The use of exogenous melatonin in delayed sleep phase disorder: a meta-analysis. Sleep 2010;33(12):1605-14
https://pubmed.ncbi.nlm.nih.gov/21120122[143] Barrett JR, Tracy DK, Giaroli G. To sleep or not to sleep: a systematic review of the literature of pharmacological treatments of insomnia in children and adolescents with attention-deficit/hyperactivity disorder. Journal of child and adolescent psychopharmacology 2013;23(10):640-7
http://dx.doi.org/10.1089/cap.2013.0059 https://pubmed.ncbi.nlm.nih.gov/24261659[144] Van der Heijden KB, Smits MG, Van Someren EJW, Ridderinkhof KR, Gunning WB. Effect of melatonin on sleep, behavior, and cognition in ADHD and chronic sleep-onset insomnia. Journal of the American Academy of Child and Adolescent Psychiatry 2007;46(2):233-41
https://pubmed.ncbi.nlm.nih.gov/17242627[145] Khan S, Heussler H, McGuire T, Dakin C, Pache D, Cooper D, Norris R, Flenady V, Charles B. Melatonin for non-respiratory sleep disorders in visually impaired children. The Cochrane database of systematic reviews 2011
http://dx.doi.org/10.1002/14651858.CD008473.pub2 https://pubmed.ncbi.nlm.nih.gov/22071850[146] Hoebert M, van der Heijden KB, van Geijlswijk IM, Smits MG. Long-term follow-up of melatonin treatment in children with ADHD and chronic sleep onset insomnia. Journal of pineal research 2009;47(1):1-7
http://dx.doi.org/10.1111/j.1600-079X.2009.00681.x https://pubmed.ncbi.nlm.nih.gov/19486273[147] Braam W, Smits MG, Didden R, Korzilius H, Van Geijlswijk IM, Curfs LMG. Exogenous melatonin for sleep problems in individuals with intellectual disability: a meta-analysis. Developmental medicine and child neurology 2009;51(5):340-9
http://dx.doi.org/10.1111/j.1469-8749.2008.03244.x https://pubmed.ncbi.nlm.nih.gov/19379289[148] Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, Vohra S, Klassen TP, Baker G. Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. BMJ (Clinical research ed.) 2006;332(7538):385-93
https://pubmed.ncbi.nlm.nih.gov/16473858[149] Guénolé F, Godbout R, Nicolas A, Franco P, Claustrat B, Baleyte J-M. Melatonin for disordered sleep in individuals with autism spectrum disorders: systematic review and discussion. Sleep medicine reviews 2011;15(6):379-87
http://dx.doi.org/10.1016/j.smrv.2011.02.001 https://pubmed.ncbi.nlm.nih.gov/21393033[150] Rossignol DA, Frye RE. Melatonin in autism spectrum disorders: a systematic review and meta-analysis. Developmental medicine and child neurology 2011;53(9):783-792
http://dx.doi.org/10.1111/j.1469-8749.2011.03980.x https://pubmed.ncbi.nlm.nih.gov/21518346[151] Malow BA, Byars K, Johnson K, Weiss S, Bernal P, Goldman SE, Panzer R, Coury DL, Glaze DG, . A practice pathway for the identification, evaluation, and management of insomnia in children and adolescents with autism spectrum disorders. Pediatrics 2012;130 Suppl 2(Suppl 2):S106-24
http://dx.doi.org/10.1542/peds.2012-0900I https://pubmed.ncbi.nlm.nih.gov/23118242[152] Fernández-San-Martín MI, Masa-Font R, Palacios-Soler L, Sancho-Gómez P, Calbó-Caldentey C, Flores-Mateo G. Effectiveness of Valerian on insomnia: a meta-analysis of randomized placebo-controlled trials. Sleep medicine 2010;11(6):505-11
http://dx.doi.org/10.1016/j.sleep.2009.12.009 https://pubmed.ncbi.nlm.nih.gov/20347389[153] van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, Kuis W, Schulpen TWJ, L'Hoir MP. Swaddling: a systematic review. Pediatrics 2007;120(4):e1097-106
https://pubmed.ncbi.nlm.nih.gov/17908730[154] Bootzin RR, Stevens SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clinical psychology review 2005;25(5):629-44
https://pubmed.ncbi.nlm.nih.gov/15953666[155] Britton WB, Bootzin RR, Cousins JC, Hasler BP, Peck T, Shapiro SL. The contribution of mindfulness practice to a multicomponent behavioral sleep intervention following substance abuse treatment in adolescents: a treatment-development study. Substance abuse 2010;31(2):86-97
http://dx.doi.org/10.1080/08897071003641297 https://pubmed.ncbi.nlm.nih.gov/20408060[156] Bei B, Byrne ML, Ivens C, Waloszek J, Woods MJ, Dudgeon P, Murray G, Nicholas CL, Trinder J, Allen NB. Pilot study of a mindfulness-based, multi-component, in-school group sleep intervention in adolescent girls. Early intervention in psychiatry 2013;7(2):213-20
http://dx.doi.org/10.1111/j.1751-7893.2012.00382.x https://pubmed.ncbi.nlm.nih.gov/22759744[157] Schregardus R. Kinderen met slaapproblemen. Amsterdam: Uitgeverij Boom
[158] Sadeh A, Mindell JA, Owens J. Why care about sleep of infants and their parents? Sleep medicine reviews 2011;15(5):335-7
http://dx.doi.org/10.1016/j.smrv.2011.03.001 https://pubmed.ncbi.nlm.nih.gov/21612956[159] Middlemiss W, Granger DA, Goldberg WA. Response to "let's help parents help themselves: a letter to the editor supporting the safety of behavioural sleep techniques". Early human development 2013;89(1):41-2
http://dx.doi.org/10.1016/j.earlhumdev.2012.07.016 https://pubmed.ncbi.nlm.nih.gov/22889752[160] Price A, Hiscock H, Gradisar M. Let's help parents help themselves: a letter to the editor supporting the safety of behavioural sleep techniques. Early human development 2013;89(1):39-40
http://dx.doi.org/10.1016/j.earlhumdev.2012.07.018 https://pubmed.ncbi.nlm.nih.gov/22883341[161] Middlemiss W, Granger DA, Goldberg WA, Nathans L. Asynchrony of mother-infant hypothalamic-pituitary-adrenal axis activity following extinction of infant crying responses induced during the transition to sleep. Early human development 2012;88(4):227-32
http://dx.doi.org/10.1016/j.earlhumdev.2011.08.010 https://pubmed.ncbi.nlm.nih.gov/21945361[162] Price AMH, Wake M, Ukoumunne OC, Hiscock H. Five-year follow-up of harms and benefits of behavioral infant sleep intervention: randomized trial. Pediatrics 2012;130(4):643-51
http://dx.doi.org/10.1542/peds.2011-3467 https://pubmed.ncbi.nlm.nih.gov/22966034[163] Boer F. Slaapproblemen bij kinderen: Kinderpsychologie in de praktijk. Lannoo-Meulenhoff Belgium 2013
[164] Karp HN. Re: a randomized, controlled trial of a behavioral intervention to reduce crying among infants. Journal of the American Board of Family Medicine : JABFM 2010;23(5):689-90; author reply 690-1
http://dx.doi.org/10.3122/jabfm.2010.05.100139 https://pubmed.ncbi.nlm.nih.gov/20823369[165] Harrington JW, Logan S, Harwell C, Gardner J, Swingle J, McGuire E, Santos R. Effective analgesia using physical interventions for infant immunizations. Pediatrics 2012;129(5):815-22
http://dx.doi.org/10.1542/peds.2011-1607 https://pubmed.ncbi.nlm.nih.gov/22508924[166] de Bruin E, Waterman D, Meijer AM. SlimSlapen: Cognitieve gedragstherapie voor insomnia (CGT-i) bij adolescenten. In: Braet C, Bögels S, eds. Protocollaire behandelingen voor kinderen en adolescenten met psychische klachten. 1st ed. Amsterdam: Boom 2013
[167] Vlasblom E, Beltman M. Rapportage Praktijktest richtlijn Gezonde slaap en slaapproblemen bij kinderen. 2016
http://dx.doi.org/TNO,%20Leiden[168] Krom M. De relatie tussen de slaapduur en het werkgeheugen van kinderen van 8-9 jaar en kinderen van 10-11 jaar oud. 2012
http://dx.doi.org/Universiteit%20Leiden[169] LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics 2005;115(1 Suppl):257-65
https://pubmed.ncbi.nlm.nih.gov/15866860[170] Meijer AM. Chronic sleep reduction, functioning at school and school achievement in preadolescents. Journal of sleep research 2008;17(4):395-405
http://dx.doi.org/10.1111/j.1365-2869.2008.00677.x https://pubmed.ncbi.nlm.nih.gov/19021856[171] Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension on sleep and cognitive performance in adolescents with chronic sleep reduction: an experimental study. Sleep medicine 2013;14(6):510-7
http://dx.doi.org/10.1016/j.sleep.2013.01.012 https://pubmed.ncbi.nlm.nih.gov/23523432[172] Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension and sleep hygiene advice on sleep and depressive symptoms in adolescents: a randomized controlled trial. Journal of child psychology and psychiatry, and allied disciplines 2014;55(3):273-83
http://dx.doi.org/10.1111/jcpp.12157 https://pubmed.ncbi.nlm.nih.gov/24252173[173] Dewald-Kaufmann JF, Oort FJ, Bögels SM, Meijer AM. Why sleep matters: Differences in daytime functioning between adolescents with low and high chronic sleep reduction and short and long sleep durations. Journal of Cognitive and Behavioral Psychotherapies 2013;13(1a):171
[174] Hunziker UA, Barr RG. Increased carrying reduces infant crying: a randomized controlled trial. Pediatrics 1986;77(5):641-8
https://pubmed.ncbi.nlm.nih.gov/3517799[175] Müller S, Hemmi MH, Wilhelm FH, Barr RG, Schneider S. Parental report of infant sleep behavior by electronic versus paper-and-pencil diaries, and their relationship to actigraphic sleep measurement. Journal of sleep research 2011;20(4):598-605
http://dx.doi.org/10.1111/j.1365-2869.2011.00926.x https://pubmed.ncbi.nlm.nih.gov/21707809[176] Werner H, Molinari L, Guyer C, Jenni OG. Agreement rates between actigraphy, diary, and questionnaire for children's sleep patterns. Archives of pediatrics & adolescent medicine 2008;162(4):350-8
http://dx.doi.org/10.1001/archpedi.162.4.350 https://pubmed.ncbi.nlm.nih.gov/18391144[177] Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, Morin CM. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep 2012;35(2):287-302
http://dx.doi.org/10.5665/sleep.1642 https://pubmed.ncbi.nlm.nih.gov/22294820[178] Erickson JM. Approaches to measure sleep-wake disturbances in adolescents with cancer. Journal of pediatric nursing 2009;24(4):255-69
http://dx.doi.org/10.1016/j.pedn.2008.03.004 https://pubmed.ncbi.nlm.nih.gov/19632503[179] Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, Martin JL. Evidence for the validity of a sleep habits survey for adolescents. Sleep 2003;26(2):213-6
https://pubmed.ncbi.nlm.nih.gov/12683482[180] Bruni O, Alonso-Alconada D, Besag F, Biran V, Braam W, Cortese S, Moavero R, Parisi P, Smits M, Van der Heijden K, Curatolo P. Current role of melatonin in pediatric neurology: clinical recommendations. European journal of paediatric neurology : EJPN : official journal of the European Paediatric Neurology Society 2015;19(2):122-33
http://dx.doi.org/10.1016/j.ejpn.2014.12.007 https://pubmed.ncbi.nlm.nih.gov/25553845[181] Cohen D, Bonnot O, Bodeau N, Consoli A, Laurent C. Adverse effects of second-generation antipsychotics in children and adolescents: a Bayesian meta-analysis. Journal of clinical psychopharmacology 2012;32(3):309-16
http://dx.doi.org/10.1097/JCP.0b013e3182549259 https://pubmed.ncbi.nlm.nih.gov/22544019[182] Owens JA, Moturi S. Pharmacologic treatment of pediatric insomnia. Child and adolescent psychiatric clinics of North America 2009;18(4):1001-16
http://dx.doi.org/10.1016/j.chc.2009.04.009 https://pubmed.ncbi.nlm.nih.gov/19836701[183] Cheng JYW, Chen RYL, Ko JSN, Ng EML. Efficacy and safety of atomoxetine for attention-deficit/hyperactivity disorder in children and adolescents-meta-analysis and meta-regression analysis. Psychopharmacology 2007;194(2):197-209
https://pubmed.ncbi.nlm.nih.gov/17572882[184] Cortese S, Holtmann M, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Dittmann RW, Graham J, Taylor E, Sergeant J, . Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents. Journal of child psychology and psychiatry, and allied disciplines 2013;54(3):227-46
http://dx.doi.org/10.1111/jcpp.12036 https://pubmed.ncbi.nlm.nih.gov/23294014[185] Fietta P, Fietta P, Delsante G. Central nervous system effects of natural and synthetic glucocorticoids. Psychiatry and clinical neurosciences 2009;63(5):613-22
http://dx.doi.org/10.1111/j.1440-1819.2009.02005.x https://pubmed.ncbi.nlm.nih.gov/19788629[186] Owens JA, Babcock D, Blumer J, Chervin R, Ferber R, Goetting M, Glaze D, Ivanenko A, Mindell J, Rappley M, Rosen C, Sheldon S. The use of pharmacotherapy in the treatment of pediatric insomnia in primary care: rational approaches. A consensus meeting summary. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2005;1(1):49-59
https://pubmed.ncbi.nlm.nih.gov/17561616[187] Kempler L, Sharpe L, Miller CB, Bartlett DJ. Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? A systematic review and meta-analysis of randomised controlled trials. Sleep medicine reviews 2016;29():15-22
http://dx.doi.org/10.1016/j.smrv.2015.08.002 https://pubmed.ncbi.nlm.nih.gov/26555938[188] Douglas PS. High level evidence does not support first wave behavioural approaches to parent-infant sleep Sleep Medicine Reviews 2015;29():
[189] Douglas P, Whittingham K. Response to 'sleeping like a baby? infant sleep: Impact on care givers and current controversies'. Journal of paediatrics and child health 2015;51(2):234
http://dx.doi.org/10.1111/jpc.12835 https://pubmed.ncbi.nlm.nih.gov/25677489[190] Gradisar M, Jackson K, Spurrier NJ, Gibson J, Whitham J, Williams AS, Dolby R, Kennaway DJ. Behavioral Interventions for Infant Sleep Problems: A Randomized Controlled Trial. Pediatrics 2016;137(6):
http://dx.doi.org/10.1542/peds.2015-1486 https://pubmed.ncbi.nlm.nih.gov/27221288[191] Hiscock H, Fisher J. Sleeping like a baby? Infant sleep: impact on caregivers and current controversies. Journal of paediatrics and child health 2015;51(4):361-4
http://dx.doi.org/10.1111/jpc.12752 https://pubmed.ncbi.nlm.nih.gov/25293637[192] Middlemiss W, Yaure R, Huey EL. Translating research-based knowledge about infant sleep into practice. Journal of the American Association of Nurse Practitioners 2015;27(6):328-37
http://dx.doi.org/10.1002/2327-6924.12159 https://pubmed.ncbi.nlm.nih.gov/25088326[193] Narvaez D. The Ethics of Early Life Care: The Harms of Sleep Training Clinical Lactation 2013;4(2):66
[194] Crncec R, Matthey S, Nemeth D. Infant sleep problems and emotional health: A review of two behavioural approaches Journal of Reproductive and Infant Psychology 2010;28(1):44
[195] Blunden SL, Thompson KR, Dawson D. Behavioural sleep treatments and night time crying in infants: challenging the status quo. Sleep medicine reviews 2011;15(5):327-34
http://dx.doi.org/10.1016/j.smrv.2010.11.002 https://pubmed.ncbi.nlm.nih.gov/21295501[196] Barlow J, National Scientific Council on the Developing Child. Excessive stress disrupts the development of brain architecture. Journal of Children's Services 2014;9(2):143
[197] Ha T, Granger DA. Family Relations, Stress, and Vulnerability: Biobehavioral Implications for Prevention and Practice Family Relations 2016;65(1):9
[198] Jansen J, Beijers R, Riksen-Walraven M, de Weerth C. Cortisol reactivity in young infants. Psychoneuroendocrinology 2010;35(3):329-38
http://dx.doi.org/10.1016/j.psyneuen.2009.07.008 https://pubmed.ncbi.nlm.nih.gov/19651476[199] Beijers R, Jansen J, Riksen-Walraven M, de Weerth C. Attachment and infant night waking: a longitudinal study from birth through the first year of life. Journal of developmental and behavioral pediatrics : JDBP 2011;32(9):635-43
http://dx.doi.org/10.1097/DBP.0b013e318228888d https://pubmed.ncbi.nlm.nih.gov/21743349[200] Bélanger M-È, Bernier A, Simard V, Bordeleau S, Carrier J. Viii. Attachment and sleep among toddlers: disentangling attachment security and dependency. Monographs of the Society for Research in Child Development 2015;80(1):125-40
http://dx.doi.org/10.1111/mono.12148 https://pubmed.ncbi.nlm.nih.gov/25704739[201] Higley E, Dozier M. Nighttime maternal responsiveness and infant attachment at one year. Attachment & human development 2009;11(4):347-63
http://dx.doi.org/10.1080/14616730903016979 https://pubmed.ncbi.nlm.nih.gov/19603300[202] McNamara P, Belsky J, Fearon P. Infant sleep disorders and attachment: Sleep problems in infants with insecure-resistant versus insecure-avoidant attachments to mother. Sleep Hypnosis 2003;5(1):17
[203] Morrell J, Steele H. The role of attachment security, temperament, maternal perception, and care-giving behavior in persistent infant sleeping problems Infant mental health journal 2003;24(5):447
[204] Mileva-Seitz VR, Luijk MPCM, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Jaddoe VWV, Hofman A, Verhulst FC, Tiemeier H. ASSOCIATION BETWEEN INFANT NIGHTTIME-SLEEP LOCATION AND ATTACHMENT SECURITY: NO EASY VERDICT. Infant mental health journal 2016;37(1):5-16
http://dx.doi.org/10.1002/imhj.21547 https://pubmed.ncbi.nlm.nih.gov/26719041[205] Pennestri M-H, Moss E, O'Donnell K, Lecompte V, Bouvette-Turcot A-A, Atkinson L, Minde K, Gruber R, Fleming AS, Meaney MJ, Gaudreau H, . Establishment and consolidation of the sleep-wake cycle as a function of attachment pattern. Attachment & human development 2015;17(1):23-42
http://dx.doi.org/10.1080/14616734.2014.953963 https://pubmed.ncbi.nlm.nih.gov/25231054[206] Zentall SR, Braungart-Rieker JM, Ekas NV, Lickenbrock DM. Longitudinal assessment of sleep–wake regulation and attachment security with parents. Infant and Child Development 2012;21(5):443
[207] Simard V, Bernier A, Bélanger M-È, Carrier J. Infant attachment and toddlers' sleep assessed by maternal reports and actigraphy: different measurement methods yield different relations. Journal of pediatric psychology 2013;38(5):473-83
http://dx.doi.org/10.1093/jpepsy/jst001 https://pubmed.ncbi.nlm.nih.gov/23428653[208] Cronin A, Halligan SL, Murray L. Maternal psychosocial adversity and the longitudinal development of infant sleep. Infancy 2008;13(5):469
[209] Sheridan A, Murray L, Cooper PJ, Evangeli M, Byram V, Halligan SL. A longitudinal study of child sleep in high and low risk families: relationship to early maternal settling strategies and child psychological functioning. Sleep medicine 2013;14(3):266-73
http://dx.doi.org/10.1016/j.sleep.2012.11.006 https://pubmed.ncbi.nlm.nih.gov/23337072[210] Morrell J, Cortina-Borja M. The developmental change in strategies parents employ to settle young children to sleep, and their relationship to infant sleeping problems, as assessed by a new questionnaire: the Parental Interactive Bedtime Behaviour Scale Infant and Child Development 2002;11(1):17
[211] Cowie J, Palmer CA, Hussain H, Alfano CA. Parental Involvement in Infant Sleep Routines Predicts Differential Sleep Patterns in Children With and Without Anxiety Disorders. Child psychiatry and human development 2016;47(4):636-46
http://dx.doi.org/10.1007/s10578-015-0597-0 https://pubmed.ncbi.nlm.nih.gov/26493392[212] Teti DM, Kim B-R, Mayer G, Countermine M. Maternal emotional availability at bedtime predicts infant sleep quality. Journal of family psychology : JFP : journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2010;24(3):307-15
http://dx.doi.org/10.1037/a0019306 https://pubmed.ncbi.nlm.nih.gov/20545404[213] Philbrook LE, Hozella AC, Kim B-R, Jian NI, Shimizu M, Teti DM. Maternal emotional availability at bedtime and infant cortisol at 1 and 3 months. Early human development 2014;90(10):595-605
http://dx.doi.org/10.1016/j.earlhumdev.2014.05.014 https://pubmed.ncbi.nlm.nih.gov/25128871[214] Hubbard FO, Van IJzendoorn MH. Maternal unresponsiveness and infant crying across the first 9 months: A naturalistic longitudinal study Infant Behavior and Development 1991;14(3):299
[215] van IJzendoorn MH, Hubbard FO. Are infant crying and maternal responsiveness during the first year related to infant-mother attachment at 15 months? Attachment & human development 2000;2(3):371-91
https://pubmed.ncbi.nlm.nih.gov/11708224[216] Hauck YL, Hall WA, Dhaliwal SS, Bennett E, Wells G. The effectiveness of an early parenting intervention for mothers with infants with sleep and settling concerns: a prospective non-equivalent before-after design. Journal of clinical nursing 2012;21(1-2):52-62
http://dx.doi.org/10.1111/j.1365-2702.2011.03734.x https://pubmed.ncbi.nlm.nih.gov/21649763[217] Whittingham K, Douglas P. Optimizing parent-infant sleep from birth to 6 months: a new paradigm. Infant mental health journal 2014;35(6):614-23
http://dx.doi.org/10.1002/imhj.21455 https://pubmed.ncbi.nlm.nih.gov/25798510[218] Mileva-Seitz VR, Bakermans-Kranenburg MJ, Battaini C, Luijk MPCM. Parent-child bed-sharing: The good, the bad, and the burden of evidence. Sleep medicine reviews 2017;32():4-27
http://dx.doi.org/10.1016/j.smrv.2016.03.003 https://pubmed.ncbi.nlm.nih.gov/27107752[219] Volkovich E, Ben-Zion H, Karny D, Meiri G, Tikotzky L. Sleep patterns of co-sleeping and solitary sleeping infants and mothers: a longitudinal study. Sleep medicine 2015;16(11):1305-1312
http://dx.doi.org/10.1016/j.sleep.2015.08.016 https://pubmed.ncbi.nlm.nih.gov/26498228[220] Tollenaar MS, Beijers R, Jansen J, Riksen-Walraven JMA, de Weerth C. Solitary sleeping in young infants is associated with heightened cortisol reactivity to a bathing session but not to a vaccination. Psychoneuroendocrinology 2012;37(2):167-77
http://dx.doi.org/10.1016/j.psyneuen.2011.03.017 https://pubmed.ncbi.nlm.nih.gov/21530088[221] Beijers R, Riksen-Walraven JM, de Weerth C. Cortisol regulation in 12-month-old human infants: associations with the infants' early history of breastfeeding and co-sleeping. Stress (Amsterdam, Netherlands) 2013;16(3):267-77
http://dx.doi.org/10.3109/10253890.2012.742057 https://pubmed.ncbi.nlm.nih.gov/23116166[222] Waynforth D. The influence of parent-infant cosleeping, nursing, and childcare on cortisol and SIgA immunity in a sample of British children. Developmental psychobiology 2007;49(6):640-8
https://pubmed.ncbi.nlm.nih.gov/17680611[223] Lucas-Thompson R, Goldberg WA, Germo GR, Keller MA, Davis EP, Sandman CA. Sleep Arrangements and Night Waking at 6 and 12 Months in Relation to Infants' Stress-induced Cortisol Responses Infant and Child Development 2009;18(6):521
1 Inleiding
De JGZ richtlijn “Gezonde slaap en slaapproblemen bij kinderen” is gericht op het bevorderen van gezond slaapgedrag en het verminderen van slaapproblemen bij kinderen van 0-18 jaar waarover vragen zijn bij ouders, de jeugdige zelf en/of professionals.
Bij JGZ-professionals bestaat behoefte aan kennis en vaardigheden om gezond slaapgedrag te stimuleren en slaapproblemen te voorkomen of te verminderen. Dat houdt in: adviezen, gebaseerd op wetenschappelijke evidentie en consensus, waar JGZ-professionals en hun cliënten mee uit de voeten kunnen. De adviezen moeten goed aansluiten bij de behoeften van ouders en kind, en passen bij de visie van ouders op de zorg voor hun kind.
2 Definities en achtergrondinformatie
2.1 Gezonde slaap
Deze subsectie geeft een introductie van de slaapopbouw, het slaapritme en de ontwikkeling van de slaap per leeftijdsfase.
2.1.1 Normaal slaapgedrag
Slaap is een normale, periodiek optredende toestand van rust, die gepaard gaat met een verlaging van het bewustzijn, waarbij het lichaam en de geest tot rust komen. Wat normaal slaapgedrag is, is onder andere afhankelijk van de leeftijd van het kind. Het slaapgedrag van een volwassene verschilt veel van het slaapgedrag van een baby. Dit hoofdstuk geeft een overzicht van de ontwikkeling in het slaapgedrag van baby’s tot en met de adolescentie. In dit hoofdstuk behandelen we de slaapopbouw per leeftijdscategorie en daarnaast ook het slaapritme en de biologische klok.
2.1.2 Slaapopbouw
Slaap bestaat uit verschillende fasen en is gericht op lichamelijk en psychisch herstel. Anders dan bij baby’s, zijn er bij kinderen en volwassenen een aantal slaapfases te onderscheiden in een slaapcyclus. Dit valt onder te verdelen in grofweg twee soorten slaap: de REM slaap (Rapid Eye Movement, actieve slaap) en de non-REM slaap (oppervlakkige en diepe slaap). Tijdens de REM slaap komt dromen veelvuldig voor en hoewel de spieren in het lichaam volledig ontspannen zijn, bewegen de ogen heen en weer (vandaar de naam “Rapid Eye Movement”). De non-REM slaap is nog onder te verdelen in lichte non-REM slaap (fase 1 en 2) en diepe non-REM slaap (fase 3).
Tijdens de slaap wisselen deze fases elkaar af: van lichte non-REM slaap, naar diepe non-REM slaap, terug naar lichte non-REM slaap en vervolgens de REM slaap. Dan begint de slaapcyclus weer opnieuw of wordt de persoon wakker. Het is normaal dat kinderen en volwassenen tussen slaapcycli enkele malen per nacht kort wakker worden, maar dat meestal niet opmerken. Per slaapperiode doorloopt een persoon een aantal slaapcycli, waarbij een slaapcyclus van een volwassene ongeveer anderhalf uur duurt.
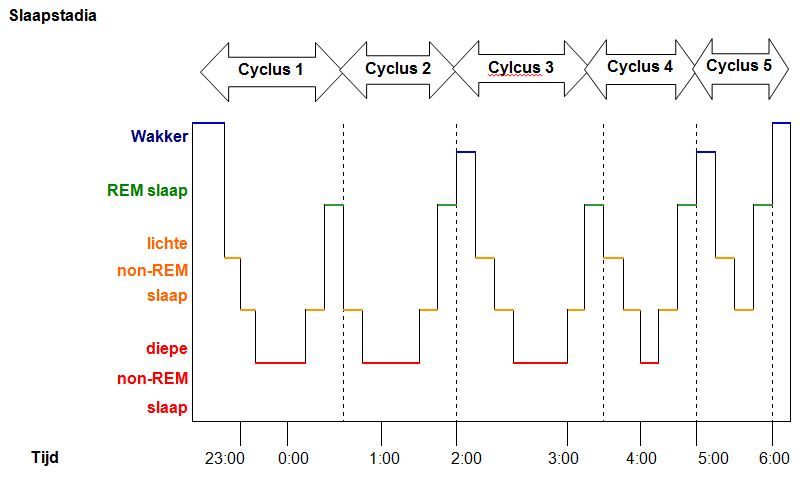
Figuur 1. Voorbeeld van de opbouw van de slaapstadia en cycli gedurende een nacht.
Slaap bij baby’s (0-6 maanden)
Baby’s hebben twee slaapfasen in een slaapcyclus: actieve slaap en stille slaap, en zij doorlopen kortere slaapcycli dan volwassenen. Tijdens de eerste zes maanden duurt een slaapcyclus zo’n 50 tot 60 minuten. Eerst hebben baby’s de actieve slaap, dit is het equivalent van de REM slaap bij volwassenen. In deze slaapfase kunnen baby’s bewegen, lachen of zelfs geluidjes maken en ademen zij snel en onregelmatig. Snelle oogbewegingen treden regelmatig op. In dit stadium slapen baby’s vrij oppervlakkig, en zij komen tijdens deze actieve slaap wat meer aan de ‘oppervlakte’ dan volwassenen (ogen gaan soms half open, kind beweegt of maakt geluid). Kinderen kunnen in de actieve fase soms bijna wakker lijken. Hierdoor kan het voor ouders soms lastig zijn om te herkennen of een kind al uitgeslapen is of nog verder zal slapen.
Ongeveer halverwege de slaapcyclus gaat de actieve slaap over in de stille slaap. Tijdens de stille slaap beweegt het kind nauwelijks. De ademhaling is rustig en regelmatig. Baby’s in stille slaap worden minder snel wakker door geluid en andere omgevingsfactoren. Na afloop van de stille slaap, wat tevens het einde is van de slaapcyclus, wordt een baby wakker, of beginnen zij de slaapcyclus weer opnieuw. De slaap-waakcyclus van een pasgeborene kent geen dag- en nachtritme, maar is ongeveer gelijk verdeeld over 24 uur (zie Figuur 2).
Slaap bij jonge kinderen (6 maanden – 4 jaar)
Naarmate baby’s ouder worden, gaat de stille slaap steeds meer over in de non-REM slaap. Dit begint op de leeftijd van 6 maanden. In de loop van het eerste levensjaar komt een dag- en nachtritme geleidelijk op gang. Deze verschuiving wordt vooral veroorzaakt door de rijping van de hersenen, maar in de loop van de maanden gaan omgevingsfactoren ook een rol spelen. Daarnaast wordt een slaapcyclus steeds langer en brengen kinderen relatief minder tijd door in de actieve slaap of REM slaap. In vergelijking met volwassenen brengen jonge kinderen veel meer tijd door in de REM slaap. Bij baby’s bestaat de slaap nog voor ongeveer de helft uit de actieve (REM) slaap, bij driejarigen is dit nog ongeveer 30%, terwijl bij volwassenen slechts ongeveer 20% van de slaap uit REM slaap bestaat.
Slaap bij kinderen (4-12 jaar)
Op de leeftijd van vier jaar duurt een slaapcyclus ongeveer 90-100 minuten. Op de leeftijd van 5 jaar loopt het percentage REM slaap terug naar ongeveer 18,5%.
Slaap bij adolescenten (vanaf 12 jaar)
Het percentage REM slaap blijft min of meer hetzelfde (18,5%) tot in de adolescentie. Dan neemt het percentage REM slaap weer toe naar ongeveer 22%. Vervolgens neemt de REM slaap in de volwassen leeftijd weer iets af naar 20% en bij ouderen (70+) zelfs naar een percentage van 14%.
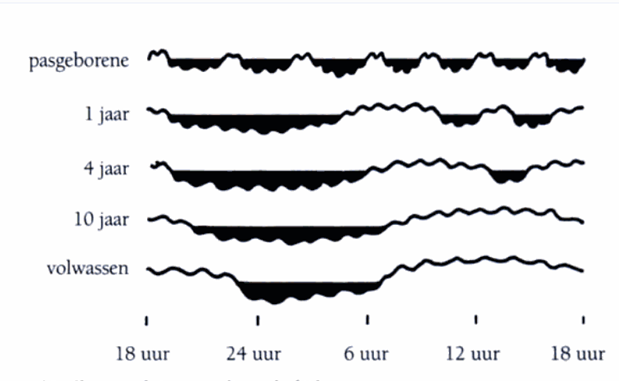
Figuur 2: Ontwikkeling van een dag-nachtritme op verschillende leeftijden (bron: Verhulst, 2005). De lijn staat voor de verschillende slaap- en waakperiodes gedurende 24 uur: Onder het zwarte vlak is men in slaap, boven het zwarte vlak is men wakker. De kleine schommelingen in de lijn symboliseren de verschillende slaapfases (afwisselend diepe en oppervlakkige slaap) en waakfases (afwisselend periodes van alertheid en van verminderde concentratie).
2.1.3 Slaapritme en de biologische klok
Hieronder wordt uitgelegd waarom mensen vooral ’s nachts slapen en overdag wakker zijn en waarom de biologische klok belangrijk is voor dit slaapritme. De slaap-waakregulatie wordt vaak beschreven volgens het Twee-processen model. Dit model beschrijft hoe slaap en waak worden bepaald door de samenwerking van twee onderling onafhankelijke processen:
- Proces S, de homeostatische slaapdruk.
De homeostatische slaapdruk houdt in dat de neiging tot inslapen stijgt naarmate men langer wakker is en meer actief is en deze daalt na voldoende slaap. Toch is het niet zo dat we op elk moment van de dag of nacht kunnen slapen om de homeostatische slaapdruk te verminderen. En op elk moment weer wakker worden als de homeostatische slaapdruk voldoende is gedaald. Dit komt door de invloed van proces C, waardoor volwassenen meestal slapen volgens een vast ritme dat zich elke 24 uur herhaalt. - Proces C, de circadiane slaapdruk.
De circadiane slaapdruk beïnvloedt de slaap zo dat ’s nachts de behoefte toeneemt om te slapen en overdag de behoefte toeneemt om wakker te zijn. Dit wordt ook wel het dag-nachtritme genoemd. Het dag-nachtritme wordt bepaald door: a) interne processen en b) omgevingsinvloeden. Beide processen worden hieronder toegelicht. Aansluitend zullen we ingaan op het ultradiane ritme (korte cycli van alertheid en verminderde concentratie binnen 24 uur).
Interne processen
De interne aansturing van het dag-nachtritme gebeurt door een kern in de hersenen, de nucleus suprachiasmaticus, ook wel de biologische klok genoemd. Deze kern is belangrijk voor de aansturing van het dag-nachtritme en de hormoonhuishouding. De kern werkt in principe zonder externe sturing. Dat betekent dat ook zonder daglicht een mens automatisch een dag-nachtritme zou kunnen volgen. Het interne dag-nachtritme duurt uit zichzelf ongeveer 25 uur. Maar onder invloed van met name licht wordt de biologische klok gesynchroniseerd met het ritme van de 24-uursdag, en met bijvoorbeeld de tijdzone of het klimaat waarin je je bevindt.
Omgevingsinvloeden
Van de omgevingsinvloeden die het dag-nachtritme beïnvloeden is licht de belangrijkste. Licht geeft via een zenuwbaan die door de oogzenuw loopt, de tractus retinohypothalamicus, een signaal aan de bovengenoemde kern in de hersenen (zie figuur 3). Deze geeft signalen door aan andere kernen in de hypothalamus, en samenhangende klieren voor productie van de hormonen cortisol en melatonine. Deze hormonen spelen een belangrijke rol in de regeling van slapen en waakzaamheid. Cortisol, ook wel het stresshormoon genoemd, maakt je wakker en actief. Cortisolniveaus zijn het hoogst in de ochtend, en dalen naarmate de dag vordert. Melatonine, het hormoon dat in de avond en nacht wordt aangemaakt, maakt je slaperig. De melatonineproductie wordt geremd door licht. Het melatonine niveau is overdag dan ook laag en begint te stijgen in de avond, als het langzaam schemerig wordt. Het melatonine niveau piekt in het midden van de nacht, en daalt daarna weer.
Het ultradiane ritme
Onder het ultradiane ritme wordt verstaan dat er binnen het 24-uurs ritme kortere cycli zijn van alertheid en verminderde concentratie. Het bepaalt dat je niet alleen aan het begin van de nacht slaperig wordt, maar ook in het begin van de middag, de after-lunch of post-pandriale dip, die plaatsvindt onafhankelijk van of er wel of niet lunch wordt gebruikt. Een ander voorbeeld van het ultradiane ritme is de Basis Rust ActiviteitsCyclus (BRAC), met een cyclus van ongeveer 1,5 uur. Deze bepaalt dat mensen ’s nachts slaapcycli hebben van ongeveer 1,5 uur met diepe en actieve slaap. Maar ook dat mensen overdag na een uur van volle concentratie vaak een wat minder alerte periode hebben.

Figuur 3. Invloed van licht op de biologische klok. De aanwezigheid van licht geeft via het oog (retina) en de tractus retinohypothalamicus (een zenuwbaan die door de oogzenuw (nervus opticus) loopt) een signaal af aan de biologische klok (nucleus suprachiasmaticus). Via de hypothalamus, de hypofyse (niet afgebeeld) en de epifyse wordt de aanmaak van melatonine en cortisol beïnvloed, wat vervolgens weer signalen zijn voor de rest van het lichaam (Bron: Abbott, 2003).
2.1.4 Slaapduur
In dit onderdeel wordt de ontwikkeling in de slaapduur per leeftijdscategorie beschreven. De behoefte aan slaap neemt af in de loop van de ontwikkeling. Er zijn veel onderzoeken gedaan die de gemiddelde slaapduur met standaarddeviaties per leeftijd beschrijven. In Tabel 1 en Figuur 4 wordt per leeftijdscategorie een overzicht gegeven van de slaapduur die in verschillende studies werd onderzocht. Deze tijden voor slaapduur zijn echter geen aanbeveling.[1]
Slaapgedrag van kinderen en ook de slaapduur is van veel factoren afhankelijk. Het is daarom lastig te bepalen wat hierin normaal en voldoende is. Voor ouders en jeugdigen zelf is het belangrijk om te weten dat er individuele verschillen zijn in slaapduur. Een bepaalde slaapduur kan voor het ene kind te kort zijn, en voor het andere kind te lang. Wat voor een kind voldoende slaap is, is niet altijd makkelijk vast te stellen, maar er zijn wel hulpmiddelen (zie ook Sectie Signalering en beoordeling van slaapproblemen).
Ouders kunnen met name op de ochtend letten, want een kind krijgt waarschijnlijk voldoende slaap, wanneer:
- het door de week ’s ochtends spontaan wakker wordt;
- het in weekeinden en vakanties niet veel later wakker wordt dan door de week (mits het de avond ervoor niet heel veel later naar bed is gegaan);
- wanneer het binnen een half uur na het opstaan trek heeft in ontbijt.
Het zegt niet zoveel als het kind overdag behoefte aan slaap lijkt te hebben. Kinderen die te weinig slapen, zijn lang niet altijd slaperiger. Soms zijn ze vooral drukker.[2]
Tabel 1. Gemiddelde slaapduur en slaapgedrag op leeftijd 0-12 jaar overgenomen uit artikel van Galland, Taylor, Elder, & Herbison.[3] Percentage van (Zwitserse) kinderen dat overdag slaapt en de slaapduur op leeftijd 13-16 jaar overgenomen uit artikel Iglowstein, Jenni, Molinari, & Largo.[4]
| Leeftijd | Gemiddelde slaapduur (range of standaarddeviatie) in uren | Gemiddeld aantal keer ’s nachts wakker worden (range) | Gemiddeld maximale duur van aaneengesloten slaap (range) | Gemiddeld aantal dutjes overdag | % kinderen dat overdag slaapt |
| 0-2 maanden | 14,6 (9,3-20) | 1,7 (0-3,4) | 5,7 (1,8-9,6) | 3,1 (1,2-5) | 100 |
| ≈ 3 maanden | 13,6 (9,4-17,8) | 0,8 (0-3) | 5,7 (1,8-9,6) | 3,1 (1,2-5) | 100 |
| ≈ 6 maanden | 12,9 (8,8-17) | 0,8 (0-3) | 8,3 (3-13,7) | 2,2 (0,9-3,5) | 100 |
| ≈ 9 maanden | 12,6 (9,4-15,8) | 1,1 (0-3,1) | 8,3 (3-13,7) | 2,2 (0,9-3,5) | 100 |
| ≈ 12 maanden | 12,9 (10,1-15,8) | 0,7 (0-2,5) | 8,3 (3-13,7) | 1,2 (0,4-2,1) | 100 |
| ≈ 2 jaar | 12 (9,7-14,2) | 0,7 (0-2,5) | 8,3 (3-13,7) | 1,2 (0,4-2,1) | 87 |
| ≈ 3 jaar | 12 (9,7-14,2) | 50 | |||
| ≈ 4 jaar | 11,5 (9,1-13,9) | 35 | |||
| ≈ 5 jaar | 11,5 (9,1-13,9) | 8 | |||
| ≈ 6 jaar | 9,7 (8,1-11,4) | 5 | |||
| ≈ 7 jaar | 9,4 (7,9-10,8) | 1 | |||
| ≈ 8 jaar | 9,3 (7,8-10,8) | ||||
| ≈ 9 jaar | 9,3 (7,8-10,8) | ||||
| ≈ 10 jaar | 9,1 (7,6-10,7) | ||||
| ≈ 11 jaar | 9 (7,3-10,6) | ||||
| ≈ 12 jaar | 8,9 (7,6-10,8) | ||||
| ≈ 13 jaar | 9,0 (SD ± 0,7) | ||||
| ≈ 14 jaar | 8,7 (SD ± 0,7) | ||||
| ≈ 15 jaar | 8,4 (SD ± 0,7) | ||||
| ≈ 16 jaar | 8,1 (SD ± 0,7) |
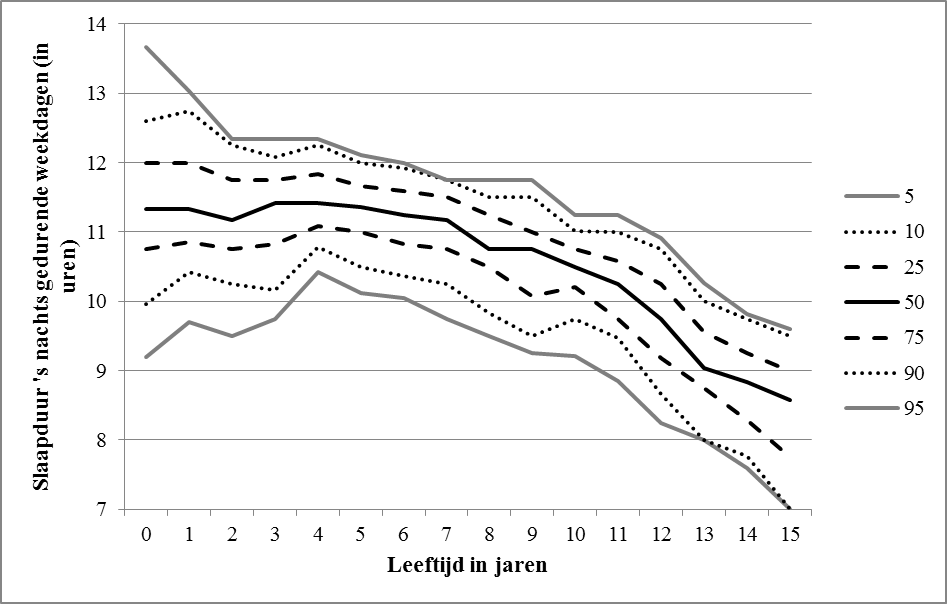
Figuur 4. Cross-sectionele gemiddelde slaaptijden van Nederlandse kinderen tijdens de nacht, tijdens weekdagen, verdeeld in percentielen (nog niet gepubliceerde data van Van der Heijden).
Baby’s (0-6 maanden)
Het leven van een pasgeboren baby bestaat voor een groot deel uit slapen. Een pasgeboren baby slaapt veel overdag en ’s nachts. Gemiddeld zo’n 14 uur per 24 uur (zie Tabel 1).[5] Doordat een pasgeboren baby vaak voeding nodig heeft, slaapt een baby niet lang achter elkaar door. Overdag slaapt een baby meestal 2,5 tot 4 uur achter elkaar. Naarmate baby’s ouder worden, worden de slaapperioden steeds langer. Vanaf ongeveer 10-12 weken begint een dag- en nachtpatroon te ontstaan.[3] Vooral de slaap in de avond en nacht wordt langer en dieper. Ongeveer 7 van de 10 baby’s slapen ’s nachts door als ze 6 maanden oud zijn (doorslapen is minimaal 5 uur achter elkaar slapen).[6] De baby slaapt ongeveer 3 tot 5 slaapcycli achter elkaar per slaapperiode
Peuters/kleuters (6 maanden tot 4 jaar)
Hoe ouder kinderen worden, hoe minder slaap ze nodig hebben (zie Tabel 1 en Figuur 4). Dit verandert van ongeveer 14 uur per dag als ze pas geboren zijn, naar ongeveer 10 uur op de leeftijd van 6 jaar. Langzaam aan leren kinderen ’s nachts doorslapen, gemiddeld vanaf 6 maanden. Kinderen van 1 jaar oud slapen ongeveer 8-9 uur aaneengesloten door. Een peuter/kleuter slaapt in de nacht ongeveer 10-12 uur. Sommige kinderen van 4 jaar oud die naar school gaan hebben nog behoefte aan slaap overdag. Uit gegevens van Zwitserse kinderen blijkt dat ongeveer één op de drie kinderen van 4 jaar oud behoefte heeft aan slaap overdag.[4]
Kinderen (4 jaar-12 jaar)
Uit Nederlands onderzoek bij kinderen van 2-14 jaar blijkt dat kinderen in Nederland gemiddeld om 8 uur naar bed gaan, en gemiddeld om 7 uur opstaan.[7] Hoe ouder de kinderen worden, hoe later zij naar bed gaan en hoe later zij opstaan. De gemiddelde totale slaapduur neemt af met de leeftijd. Het gemiddeld aantal minuten dat kinderen ’s nachts wakker zijn, was in de Nederlandse studie gemiddeld 8 minuten in totaal per nacht, en dit was niet gerelateerd aan de leeftijd. Uit ander onderzoek bij Nederlandse kinderen van 7- 12 jaar blijkt dat er geen verschil is tussen de slaapduur door de week en in het weekend. Echter, het middelpunt van de slaap ligt in het weekend later dan doordeweeks.[8]
Adolescenten (12 jaar-18 jaar)
Adolescenten vanaf 12 jaar hebben ongeveer 9 uur slaap nodig. Op de leeftijd van 18 jaar loopt dit terug naar ongeveer 8,5 uur. Bij adolescenten is het opvallend dat zij tussen de leeftijd van 14 en 18 meer REM slaap nodig hebben dan kinderen van 5- 13 jaar en ook meer dan volwassenen van boven de 30 jaar oud.
Bovendien vindt aan het begin van de puberteit een verschuiving plaats van het biologische klokritme naar een later tijdstip. Tijdens de adolescentie verschuift het slaapritme ongeveer twee tot drie uur.[9] Dit betekent dat pubers naarmate zij ouder worden, pas een paar uur later in slaap kunnen vallen. Dit kan niet voldoende worden gecompenseerd door elke dag op hetzelfde (vroege) tijdstip naar bed te gaan en op te staan. Met andere woorden; een vroeger slaapritme kan niet worden afgedwongen. Omdat adolescenten gemiddeld wel 9 uur slaap nodig hebben, kan de behoefte om uit te slapen ontstaan.
Ook is er bij adolescenten vaak meer variabiliteit tussen de slaap op schooldagen en in het weekend, waarbij adolescenten in het weekend langer slapen dan op schooldagen.[10]
Hoewel na de leeftijd van 23 jaar het ritme geleidelijk aan weer wat terug verschuift, kan het vroege opstaan voor school voor sommige pubers (die al een later ritme hadden) een probleem worden.
2.2 Slaapproblemen
Deze subsectie beschrijft de definitie van slaapproblemen en slaapstoornissen, de prevalentie en de gevolgen van slaapproblemen.
2.2.1 Definitie slaapproblemen en slaapstoornissen
Deze richtlijn richt zich op de preventie, het adequaat signaleren, en de behandeling van slaapproblemen in de JGZ en tijdige en adequate signalering en verwijzing wanneer er sprake is van een slaapstoornis. Echter, de grens tussen een slaapprobleem en een slaapstoornis is moeilijk scherp te definiëren.
Beter is een spectrum voor te stellen waarbij een gezonde, niet problematische slaap en normaal functioneren overdag aan het ene eind van het spectrum te vinden is en slaapstoornissen aan de andere kant van het spectrum. Ergens daartussenin zijn slaapproblemen te plaatsen die, als zij in ernst, frequentie en/of duur toenemen, over kunnen gaan in een slaapstoornis.
Een uitgebreide omschrijving van verschillende slaapstoornissen is beschreven in de internationale classificatie van slaapstoornissen (ICSD-3)[11] en in de diagnostische en statistische handleiding van mentale stoornissen (DSM-5).[12] Voor de JGZ professional is het belangrijk op de hoogte te zijn van de verschillende slaapstoornissen om deze te kunnen herkennen, maar het is niet de taak van de JGZ om deze stoornissen te diagnosticeren. In de sectie Signalering en beoordelen van slaapproblemen is daarom een overzicht te vinden van de meest voorkomende slaapstoornissen.
Naast de klinische diagnose van slaapstoornissen worden slaapproblemen bij jonge kinderen vaak gedefinieerd aan de hand van de problemen die ouders ervaren met het (niet-)slapen van hun kind. Er worden in de internationale literatuur twee typen slaapproblemen onderscheiden; het inslaapassociatie type en het type waarbij ouders moeite hebben met het stellen van grenzen.[13]
Bij het inslaapassociatie type heeft het kind bepaalde problematische of veeleisende omstandigheden nodig voordat het in slaap kan vallen. Bij het andere type kan de ouder onvoldoende grenzen stellen als het kind het slapen probeert uit te stellen of naar bed weigert te gaan. In deze definitie van slaapproblemen wordt echter geen rekening gehouden met andere slaapproblemen die bij kinderen kunnen voorkomen, zoals nachtmerries, snurken, slaapwandelen, etc.
Beschrijvingen van slaapproblemen bij oudere kinderen en adolescenten zijn zeer divers en hangen vaak samen met de criteria die voor verschillende slaapstoornissen in de DSM-5 en de ICSD-3 worden gegeven.
Slaapproblemen kunnen aanhoudend of van voorbijgaande aard zijn. De meerderheid van de slaapproblemen is van tijdelijke aard en verdwijnt vanzelf na een aantal weken of maanden.[14] Ongeveer een kwart tot een derde van de slaapproblemen blijft bestaan.[15] Slaapproblemen zijn minder vaak persistent dan slaapstoornissen.[16]
2.2.2 Prevalentie van slaapproblemen
Baby’s (0-6 maanden)
Uit onderzoek bij Nederlandse baby’s van 6 maanden ervaart één op de tien ouders het slapen van hun kind als een probleem.[17] Van het totaal aantal huisartsenconsulten in Nederland voor kinderen jonger dan 1 jaar gaat het in 0,5% om slaapproblemen bij meisjes en in 1% om slaapproblemen bij jongens.[18]
Jonge kinderen (6 maanden-12 jaar)
Op de leeftijd van 0-2 jaar komen slaapproblemen vaak voor; ze behoren tot de ‘normale’ opvoedingsproblemen in deze ontwikkelingsfase.[19] Echter als de problemen in frequentie, duur of intensiteit toenemen, kunnen ze door ouders als ernstig en belemmerend worden ervaren. Prevalentiecijfers van slaapproblemen bij peuters en kleuters liggen in internationale studies tussen de 20-30%.[11] 0 Bij Nederlandse kinderen van 1,5 jaar ervaart 8% van de ouders het slapen als een probleem.[17] In een ander Nederlands onderzoek naar slaapproblemen bij kinderen van 2- 14 jaar bleek dat ongeveer een kwart van de ouders minstens 1 slaap-gerelateerd probleem ervaart.[7] Het vaakst wordt daarbij slaperigheid overdag genoemd. Bij jonge kinderen van 2-6 jaar kwam vaker dan bij oudere kinderen de volgende slaapproblemen voor: weigeren om naar bed te gaan, angst om te gaan slapen, ’s nachts wakker worden, parasomnia’s (bijvoorbeeld slaapwandelen en tandenknarsen) en problemen met ademhaling tijdens de slaap. Problemen met in slaap vallen, problemen met slaapduur en vermoeidheid overdag kwamen vaker voor bij oudere kinderen (10-14 jaar).
Adolescenten (12-18 jaar)
Bij adolescenten ligt de prevalentie van slaapproblemen, gebaseerd op internationaal onderzoek, tussen de 7 en 36%, afhankelijk van de gebruikte definities.[10] Er zijn geen prevalentiecijfers van slaapproblemen bij adolescenten uit Nederlands onderzoek bekend. Wel is bekend dat van het totaal aantal huisartsconsulten voor kinderen van 15-17 jaar het in 0,4% om slaapproblemen gaat bij meisjes en in 0,3% om slaapproblemen bij jongens.[18]
2.2.3 Gevolgen van slaapproblemen
Slaapproblemen kunnen ernstige gevolgen hebben voor zowel kinderen zelf als voor hun ouders. Hieronder worden de gevolgen van slaapproblemen per leeftijdsgroep besproken.
Baby’s (0-6 maanden)
Voor baby’s is het normaal dat zij ’s nachts vaak wakker worden, bijvoorbeeld voor een voeding. Na ongeveer 8 weken gaan baby’s gaandeweg vaker ‘s nachts een keer een voeding overslaan en langer dan 5 uur doorslapen, maar dit verschilt per kind.[6] Uit een aantal onderzoeken blijkt dat de slaap van baby’s gerelateerd is aan het temperament, de cognitieve en motorische ontwikkeling. Het is echter nog niet duidelijk of er een oorzakelijke relatie is tussen de slaapduur en het temperament en de ontwikkeling van baby’s.[21]
Bij ongeveer 20% van alle baby’s doen zich zogenaamde ‘regulatieproblemen’ (huil-, slaap- en/of voedingsproblemen) voor. In een meta-analyse van 22 longitudinale onderzoeken, met in totaal 1935 kinderen, is nagegaan of er een verband is tussen regulatieproblemen, waaronder persisterend huilen, en slaap- en eetgedrag en gedragsproblemen op latere leeftijd.[22] De resultaten laten zien dat wanneer er sprake is van regulatieproblemen in het eerste jaar (slapen, eten, huilen) de kans op gedragsproblemen later groter is. De kans is het grootst bij kinderen die meerdere regulatieproblemen tegelijk hebben en in gezinnen met meerdere psychosociale problemen
Jonge kinderen (6 maanden-4 jaar)
Slaapproblemen, een slaaptekort en daarbij behorende moeheid overdag kunnen bij jonge kinderen leiden tot emotionele/gedragsproblemen en ongevallen.[23][24][25] Slaapproblemen op jonge leeftijd zijn op latere leeftijd ook gerelateerd aan angst en depressieklachten, aandachtsproblemen en agressief gedrag.[26]
Een korte slaapduur is daarnaast ook causaal gerelateerd aan een daaropvolgende gewichtstoename bij jonge kinderen. Voor elk uur per nacht dat een kind langer slaapt, wordt het risico op overgewicht en obesitas verminderd met gemiddeld 9% (OR 0,91. 95%CI 0.84–1.00).[27]
Schoolgaande kinderen (basisschool) (4 jaar-12 jaar)
Uit een uitgebreide meta-analyse naar de relatie tussen slaap en cognitie en gedragsproblemen bij kinderen van 5-12 jaar bleek dat slaapduur een significante positieve relatie met cognitieve prestaties had.[28] Verder hangt een kortere slaapduur samen met meer gedragsproblemen, voor zowel internaliserende als externaliserende gedragsproblemen.
Chronisch slaaptekort kan ook leiden tot hyperactiviteit, in sommige gevallen kan dit lijken op ADHD.[29] Ook slaapstoornissen gaan vaak samen met substantiële gedragsproblemen en een cognitieve achterstand bij kinderen.[30] Hoewel de literatuur naar kinderen minder uitgebreid is dan bij volwassenen, ontstaan vergelijkbare tekorten in cognitief functioneren als resultaat van verstoorde slaap.
Een te korte slaapduur (dit is voor ieder kind verschillend) kan overgewicht veroorzaken bij kinderen in deze leeftijdscategorie.[31]
Adolescenten (12 jaar-18 jaar)
Bij adolescenten heeft een slaaptekort negatieve gevolgen voor de schoolprestaties en cognitief functioneren, en zien we meer depressie, angst, gedragsproblemen, risicogedrag, auto-ongelukken, roken, alcohol en drugsgebruik.[24][32][33][34][35]
Uit cross-sectionele studies blijkt dat er een associatie is tussen slaaptekort en slechte ervaren gezondheid, gewichtstoename, pijn, verhoogd cardiovasculair en cardiometabool risico, aandachtsproblemen, afzondering, agressie, geweld en suïcidale gedachten.
Wederkerige associaties zijn ook vaak beschreven, bijvoorbeeld dat slaaptekort leidt tot depressie en depressie en angst zijn sterke voorspellers voor slaapproblemen, waardoor een vicieuze cirkel ontstaat. Dit geldt ook voor pijnklachten en middelengebruik.
Uit Nederlands onderzoek onder adolescenten van 12-16 jaar blijkt dat BMI en slaapduur onderling samenhangen; wanneer in de puberteit de BMI omhoog gaat, gaat de slaapduur omlaag.[36] Ook is een kortere slaapduur gerelateerd aan een verstoorde glucosetolerantie bij adolescenten.[37]
Onderzoek toont aan dat een slaaptekort een negatieve invloed heeft op het immuunsysteem bij volwassenen.[38] Er is weinig onderzoek gedaan bij kinderen, maar bij adolescenten van 14-16 jaar werd ook een relatie aangetoond tussen korte slaapduur en ziek zijn (bijv. verkoudheid).[39]
Ouders
Slaapproblemen van kinderen kunnen ook gevolgen hebben voor de gemoedstoestand van ouders.[40][41] Slaapproblemen bij kinderen kunnen een negatief effect hebben op de mentale en fysieke gezondheidstoestand van ouders.[42] Uit onderzoek blijkt dat er een relatie is tussen slaaptekort bij kinderen, stress bij ouders, gezinsproblemen en mishandeling van kinderen.
Slapeloosheid bij ouders, bijvoorbeeld doordat hun baby ’s nachts niet slaapt en veel huilt, kan leiden tot problemen in de relatie tussen ouders.[5] Daarnaast hebben ouders van pasgeboren baby’s vaak zelf last van slaapproblemen omdat hun baby een ander slaapritme heeft en zij hun baby ’s nachts moeten voeden.[43]
3 Risico- en beschermende factoren
Factoren die samenhangen met slaap
Er zijn verschillende factoren van invloed op slaapproblemen. Zo zijn er predisponerende factoren, bijvoorbeeld een genetische aanleg, temperament, onderliggende medische aandoeningen of psychiatrische stoornissen. Daarnaast zijn er uitlokkende factoren die aan slaapproblemen vooraf gaan, zoals stress of ziekte. Ten slotte zijn er ook bestendigende factoren, zoals ongezonde slaapgewoonten, cafeïnegebruik, aangeleerde associaties die de slaap belemmeren en piekeren over slaap [33].
Voor het opsporen van problematisch slaapgedrag en het voorkomen van slaapproblemen is het van belang om de samenhangende factoren goed te kennen. Inzicht in deze factoren zal helpen bij het identificeren van kinderen die mogelijkerwijs een groter risico lopen om slaapproblemen te ontwikkelen, zodat deze kinderen en hun ouders kunnen worden ondersteund door preventieve voorlichting over slaap (zie Preventie van Slaapproblemen).
Uiteraard betekent de aanwezigheid van één of meerdere factoren niet dat er dan altijd een slaapprobleem is of zal ontstaan. En ook andersom, de afwezigheid van deze factoren betekent niet dat er geen sprake is of zal zijn van een slaapprobleem.
In deze subsectie worden voornamelijk de samenhangende factoren van slaapproblemen beschreven die in de internationale literatuur naar voren komen. Er zijn weinig Nederlandse onderzoeken naar de risico- en beschermende factoren voor slaapproblemen. Daarnaast is er geen onderzoek van voldoende kwaliteit om uitspraken te doen of deze factoren slaapproblemen daadwerkelijk veroorzaken.
Aanbevelingen
3.1 Risicofactoren
Borstvoeding van zuigelingen
Uit internationaal onderzoek blijkt dat borstvoeding is geassocieerd met minder doorslapen bij baby’s.[48][49] In een recente studie werd echter geen verschil gevonden in frequentie van ’s nachts wakker worden tussen baby’s van 6-12 maanden die borstvoeding of kunstvoeding kregen.[51] Baby’s die borstvoeding kregen, werden vaker ’s nachts gevoed dan kinderen die kunst-melkvoeding kregen, maar ze werden niet vaker wakker (zonder een voeding te krijgen). Voor ouders is het belangrijk om te weten dat als zij borstvoeding geven, het normaal is dat hun kind nog niet doorslaapt.
(Beeld)schermgebruik
Het gebruik van verschillende beeldscherm-toestellen is gerelateerd aan een korte slaapduur en later tijdstip van naar bed gaan.[52][99] Dit is gevonden voor beeldschermen in de slaapkamer, TV kijken, het gebruik van computers, gamen, internetten en het gebruik van tablets en mobiele telefoon. Veel kinderen en jongeren, en ouders zelf nemen hun telefoon of tablet mee naar de slaapkamer. Uit onderzoek blijkt dat slapen naast een klein scherm, slapen met een TV in de slaapkamer en meer schermtijd geassocieerd zijn met een kortere slaapduur.[54] Zelfs baby’s van 6 maanden die blootgesteld worden aan digitale media in de avond hebben een kortere slaapduur.[53]
Er zijn drie mogelijke verklaringen waarom beeldschermgebruik gerelateerd is aan een korte slaapduur: a) de duur van schermgebruik voor het naar bed gaan gaat direct ten koste van de slaapduur; b) de schermen geven licht af, wat het circadiane ritme verstoort doordat melatonine niet wordt aangemaakt, wat resulteert in moeite met in slaap vallen; c) schermgebruik kan door een mentale, emotionele en psychische staat van arousal (verhoogde staat van alertheid) de slaap verstoren.[100] Er is weinig experimenteel onderzoek gedaan, en wat er is gedaan is heel kleinschalig. Er is daarom onvoldoende onderzoek van voldoende kwaliteit om vast te stellen dat er een causaal verband is tussen schermgebruik en slaapproblemen.[101]
Roken
Zowel roken door adolescenten zelf [56] als passief meerokende kinderen [60] lijken vaker last te hebben van slaapproblemen. In een systematische review naar de gevolgen van roken op sociaal en gezondheidsgedrag werd één studie gevonden waarin de relatie tussen roken en slaapproblemen werd onderzocht.[56] In dit onderzoek [57] is een relatie gevonden tussen roken tijdens de adolescentie en daaropvolgende slaapproblemen waarbij gecorrigeerd werd voor leeftijd, geslacht, etnische achtergrond, en gezinsinkomen. Ook een andere studie vond dat slaperigheid overdag en slaap-waak problemen o.a. zijn gerelateerd aan roken bij adolescenten.[59] In een studie naar risicogedrag en slaap bij jongeren van gemiddeld 14 jaar bleek dat roken en slaap in het weekend bi-directioneel gerelateerd zijn. [58] In een review [60] naar de effecten van passief roken werd één relevante studie gevonden over de relatie tussen passief roken en slaap bij kinderen. De resultaten laten zien dat passief roken geassocieerd was met een langere inslaapduur, verstoorde ademhaling tijdens de slaap, parasomnia’s, vermoeidheid overdag, en algemene slaapproblemen bij kinderen van 6-12 jaar. Meer blootstelling bij jongens was gerelateerd aan meer slaapangst, terwijl meer blootstelling bij meisjes gerelateerd was aan langere inslaapduur.
3.2 Beschermende factoren
Slaaphygiëne
Een slechte slaaphygiëne is vaak de oorzaak van een slaapprobleem. Slaaphygiëne is een veelomvattend begrip en een aantal van de in dit hoofdstuk beschreven risicofactoren kunnen een onderdeel zijn van een slechte slaaphygiëne. Onder slaaphygiëne wordt een aantal gewoontes, gedragingen en omgevingsfactoren verstaan dat bijdraagt aan een regelmatige gezonde nachtrust. Het verbeteren van de slaaphygiëne kan leiden tot een verbetering van de slaap (zie Thema 4). Er is een aantal reviews waarin wordt beschreven dat een slechte slaaphygiëne gerelateerd is aan slaapproblemen. Bij kinderen van 0-10 jaar is een onvoldoende slaaphygiëne, zoals een ouder die aanwezig blijft bij inslapen, het ontbreken van een routine rondom het slapen gaan, een televisie in de slaapkamer en consumptie van cafeïne kort voor het slapen gaan, sterk geassocieerd met een korte slaapduur en slaapproblemen bij jonge kinderen.[40]
Uit een review [45] naar slaaphygiëne bij baby’s blijkt uit verschillende onderzoeken dat een routine bij het naar bed gaan baby’s helpt in slaap te vallen en angst voor separatie van de ouders reduceert. Routines kunnen bestaan uit een voeding geven, in bad gaan, voorlezen of zingen en rust voor het naar bed gaan. Het gebruik van slaaphulpmiddelen, zoals een knuffel of een fopspeen (zie ook de Handleiding Aandachtspunten Preventieve Mondzorg 0-19 jaar voor de Jeugdgezondheidszorg en de JGZ-richtlijn Preventie Wiegendood), helpt bij het reduceren van het nodig hebben van de ouders om in slaap te vallen, hoewel de kwaliteit van de studies waarin dit werd gevonden wisselend is. Een duidelijk verschil tussen dag en nacht werd geassocieerd met meer succes bij het introduceren van een slaaproutine voor bedtijd. In één observationele studie werd een mogelijke relatie tussen blootstelling aan licht overdag en de slaap ’s nachts verkend. Baby’s die meer blootgesteld werden aan daglicht in de namiddag sliepen ’s nachts beter dan baby’s die minder blootgesteld werden aan daglicht in de namiddag.
Slaaphygiëne is ook belangrijk bij adolescenten. Er is bewijs dat de volgende onderdelen van slaaphygiëne slecht zijn voor de slaap in de nacht: dutjes overdag, onregelmatige patronen van naar bed gaan en wakker worden, schermgebruik, en cognitief, sociaal of fysiek stimulerende activiteiten kort voor het slapen.[46] Ook uit Nederlands onderzoek blijkt dat er een relatie is tussen slaap hygiëne en de kwaliteit van de slaap en de slaapduur bij adolescenten.[47]
Schooltijden
Uit internationale onderzoeken waarbij de schoolaanvangstijden voor adolescenten verlaat worden, blijkt dat dit niet leidt tot andere inslaaptijden, maar wel tot meer slaap, minder vermoeidheid overdag, minder verzuim, meer tevredenheid over de slaap en afnames van zelf gerapporteerde somberheid, vermoeidheids- gerelateerde klachten etc. Bij jongere adolescenten zijn dezelfde feiten vastgesteld. Deze langere slaapduur is geassocieerd met verbeteringen in gedrag die belangrijk zijn voor aanwezigheid op school, schoolprestaties en veiligheid.[100][102] Dit komt mede omdat zonlicht een grote invloed heeft op ons biologisch slaapritme. Tijdens de adolescentie verschuift het slaapritme ongeveer drie uur. Dit kan onvoldoende worden gecompenseerd door elke dag op dezelfde tijd naar bed te gaan en op te staan (zie Thema 1). In een overzichtsstudie naar het biologische ritme van adolescenten wordt beschreven dat op de leeftijd van tien jaar, de biologische tijd van opstaan rond 06:30 is, en dat een daarmee een goed afgestemd begin van de schooltijd rond de 08:30-09:00 zou moeten liggen. Op de leeftijd van 16 is de biologische tijd van opstaan rond 08:00 uur en de bijbehorende schooltijd tussen 10:00 en 10:30. Op de leeftijd van 18 jaar is de biologische tijd van opstaan rond 09:00 uur en de gesynchroniseerde schooltijd tussen 11:00 en 11:30.[103] Er werden geen studies gevonden naar de invloed van het verschuiven van de aanvangstijden van school bij adolescenten in Nederland. Het is daarom onduidelijk in hoeverre deze tijden opgaan voor de Nederlandse situatie.
3.3 Alcohol, drugs, energiedrank
Cafeïne
De inname van cafeïne, waaronder door inname van koffie, cola, energiedrankjes, thee (behalve kruidenthee), ijsthee, chocolade en chocolademelk, is geassocieerd met een kortere slaapduur bij zowel adolescenten als jongere kinderen.[55] Er is niet veel onderzoek gedaan onder adolescenten en kinderen naar het gebruik van cafeïne en het effect op slaap. Bij volwassenen is er wel onderzoek gedaan, waaruit blijkt dat cafeïne het percentage diepe slaap vermindert en effect heeft op de REM slaap. Wel is er steeds meer wetenschappelijk bewijs dat adolescenten steeds meer cafeïne gebruiken, en dat dit mogelijk een negatief effect heeft op hun slaap. Adolescenten en kinderen denken dat het gebruik van energiedrankjes en koffie een energie-boost geeft en hen helpt om wakker te blijven. Zij zijn zich echter minder bewust van de negatieve effecten van cafeïne. De exacte richting van de relatie tussen cafeïne en slaap blijft onduidelijk: gebruiken adolescenten cafeïne omdat zij vermoeid zijn, of zijn zij vaker vermoeid omdat zij cafeïne gebruiken?[100]
Alcohol
Er werden geen reviews of meta-analyses gevonden over de relatie tussen slaap en alcohol. Wel werd een aantal artikelen gevonden waarin de relatie tussen slaap en alcohol werd onderzocht. In een prospectieve cohortstudie onder adolescenten werd aangetoond dat slaapproblemen en slaapduur significante voorspellers zijn voor alcoholgebruik.[61] In een andere studie [58] bleek dat alcoholgebruik juist kortere uitslaapduur in het weekend voorspelde. Ook de slaappatronen en slaapduur van de jongeren voorspelden alcoholgebruik. Niet alle studies vonden een relatie tussen alcohol en slaap. In een studie naar de effecten van een korte slaapduur onder kinderen van 11-17 jaar werd geen effect gevonden op alcoholgebruik. [62]
Drugs
Er werden geen reviews of meta-analyses gevonden over het effect van drugs op slaap bij kinderen. Wel werd een aantal artikelen gevonden waarin de relatie tussen slaap en drugsgebruik bij kinderen werd onderzocht. Zo is een korte slaapduur (minder dan 6 uur slaap) door de weeks gerelateerd aan drugsgebruik [62] en zijn slaapduur en slaapproblemen significante voorspellers van drugsgebruik.[61] Uit een andere studie [58] blijkt dat marihuanagebruik en totale slaapduur elkaar wederzijds negatief beïnvloeden.
4 Preventie
In Nederland zijn geen bewezen effectieve programma’s ter preventie van slaapproblemen beschikbaar. Uit internationaal onderzoek blijkt dat slaapproblemen bij jonge kinderen kunnen worden voorkomen door voorlichting aan ouders.[20][112][113][114]
Het is niet bekend welke elementen van voorlichting effectief zijn[115], maar een gezonde slaaphygiëne wordt vaak genoemd. Onder slaaphygiëne wordt een aantal gewoontes, gedragingen en omgevingsfactoren verstaan die bijdragen aan een regelmatige gezonde nachtrust. Ook bij oudere kinderen en adolescenten blijft slaaphygiëne belangrijk, hoewel voorlichting bij adolescenten niet altijd effect lijkt te hebben op het daadwerkelijke slaapgedrag.[113]
De rol van de JGZ is een preventieve, dus in eerste instantie zorgen dat slaapproblemen niet ontstaan en zorgen dat de problemen niet groter worden of zelfs afnemen. De taak van de JGZ is ouders en jeugdigen voor te lichten over normale slaap en het belang van een goede slaaphygiëne.
Aanbevelingen
4.1 0 tot 6 maanden
Aanbevelingen
4.2 6 maanden tot 4 jaar
Aanbevelingen
4.3 4 tot 12 jaar
Aanbevelingen
4.4 12 tot 18 jaar
Aanbevelingen
5 Signaleren, diagnostiek en verwijzen
De JGZ heeft een belangrijke rol bij het signaleren van kinderen met slaapproblemen en hun ouders. In dit hoofdstuk wordt besproken hoe de JGZ slaapproblemen kan signaleren, en kan beoordelen of verwijzing noodzakelijk is of dat begeleiding door de JGZ kan gebeuren.
Het stellen van de diagnose van een slaapstoornis is niet de taak van de JGZ, wel is het belangrijk om kinderen bij een vermoeden van een slaapstoornis door te verwijzen (zie Samenwerken en verwijzen).
Daarnaast is het de taak van de JGZ bij slaapproblemen zelf interventies in te zetten (zie Begeleiden en behandelen).
Aangezien slaapproblemen bij bepaalde kinderen vaker voorkomen, is het voor de JGZ van belang op de hoogte te zijn van de risicofactoren (zie Risico- en beschermende factoren).
Vragenlijsten 4 – 10 jaar
Na het stellen van de vier korte oriënterende vragen kan de JGZ professional ouders of de jongere zelf vragen om een vragenlijst in te vullen, voorafgaand aan het volgende contactmoment (zie de subsectie Gevalideerde vragenlijsten). Deze vragenlijsten kunnen een deel van de brede anamnese in de subsectie Uitgebreide vragenlijsten vervangen.
In Nederland werd de “Child Sleep Hygiëne Questionnaire” (CSHQ) onderzocht en gevalideerd bij kinderen.[125] Deze vragenlijst bestaat uit 33 vragen over slaapgewoonten en is gevalideerd voor ouders van kinderen van 4-10 jaar.
Vragenlijsten Adolescenten
Voor adolescenten zijn er twee vragenlijsten beschikbaar. De “Adolescent Sleep Hygiene Scale”(ASHQ) werd in Nederland onderzocht en gevalideerd voor adolescenten.[47] Deze vragenlijst bestaat uit 28 items over slaaphygiëne. De “Chronic Sleep Reduction Questionnaire” (CSRQ) werd eveneens onderzocht en gevalideerd voor Nederlandse adolescenten.[126] De vragenlijst bestaat uit 20 items over slaaptekorten.
Het is waarschijnlijk dat ouders en jeugdigen zelf via internet op zoek gaan naar informatie en hulp over slaapproblemen alvorens professionele hulp te zoeken. Op internet is een Nederlandse zelftest beschikbaar voor jongeren met slaapproblemen: www.slimslapen.nl/zelftest. Deze test werkt als screeningsinstrument voor “insomnia disorder” volgens de DSM-5, maar is niet wetenschappelijk onderbouwd.
Signaleren slaapstoornissen
Veel kinderen hebben geen slaapstoornis, maar een probleem in het slaapgedrag. Er is in Nederland geen voor de JGZ bruikbaar en wetenschappelijk onderbouwd en gevalideerd screeningsinstrument om slaapproblemen van slaapstoornissen te onderscheiden. Het is niet de taak van de JGZ om slaapstoornissen te diagnosticeren. Deze richtlijn richt zich op het adequaat signaleren en behandelen van slaapproblemen en tijdige en adequate signalering en verwijzing wanneer er sprake is van een slaapstoornis. Echter, de grens tussen een slaapprobleem en een slaapstoornis is moeilijk scherp te definiëren.
De werkgroep beveelt aan een spectrum voor te stellen waarbij een gezonde, niet problematische slaap en normaal functioneren overdag aan het ene eind van het spectrum te vinden is en slaapstoornissen aan de andere kant van het spectrum. Ergens daartussenin zijn slaapproblemen te plaatsen die, als zij in ernst, frequentie en/of duur toenemen, over kunnen gaan in een slaapstoornis.
In tabel 2 worden de meest voorkomende slaapstoornissen kort omschreven. De jeugdarts of verpleegkundig specialist kan hiermee de slaapstoornis niet diagnosticeren, maar het geeft wel een richting waar men aan kan denken en suggesties voor de actie die ondernomen dient te worden indien er een vermoeden van een slaapstoornis bestaat. Bij slaapstoornissen is het medisch gezien niet schadelijk wanneer het in een enkel geval niet direct onderkend wordt.
Tabel 2. Korte omschrijving van slaapstoornissen die voor kunnen komen bij kinderen en suggesties voor te ondernemen actie.
| Stoornis | Korte omschrijving | Te ondernemen actie |
| Primaire insomnie |
Onvoldoende kwaliteit of kwantiteit van slaap Minstens drie maanden lang, gedurende minstens drie nachten per week zijn er problemen met inslapen (langer dan 30 min., komt vaker voor bij adolescenten), doorslapen (meer dan drie keer per nacht wakker worden of het opnieuw in slaap vallen duurt langer dan 30 min.), te vroeg wakker worden (minimaal 30 min. vroeger dan de geplande wektijd) en/of men voelt zich niet voldoende uitgeslapen, terwijl er wel voldoende tijd was om te slapen. De slaapproblemen veroorzaken problemen in het dagelijks functioneren en worden niet veroorzaakt door andere (slaap)stoornissen, of externe factoren (bijvoorbeeld middelengebruik) |
Bij een vermoeden van een primaire insomnie kan gestart worden met een interventie in de JGZ, zie Thema 6. Indien deze na een maand nog geen effect heeft, dan doorverwijzen naar een kinderarts of een specialist in een slaapcentrum. Bij kinderen met meervoudige problematiek is mogelijk intensieve behandeling in een slaapcentrum gewenst. |
| Slaapafhankelijke ademhalingsstoornissen (sleep disordered breathing (SDB). |
Slaapafhankelijke ademhalingsstoornissen zijn bijvoorbeeld snurken en het Obstructieve Slaapapneu Syndroom (OSAS). Snurken komt bij ongeveer één op de tien kinderen voor en kan veelal worden verklaard door vergrote keel- en/of neusamandelen. Andere oorzaken kunnen een afwijkende anatomie van het KNO-gebied en hypotonie zijn. Bij OSAS is er sprake van een korte ademstilstand tijdens de slaap. Tijdens de ademstilstanden of verminderde ademhalingen, heeft de patiënt wel een prikkel om adem te halen, maar de ingeademde lucht komt niet verder dan de keel. De luchtweg is geblokkeerd. Tijdens de slaap ontspannen de spieren. Daardoor kunnen de tong en de zachte delen van het verhemelte in de keel de luchtweg blokkeren. Het is belangrijk op te merken dat bij OSAS in principe geen gevaar bestaat voor verstikking. De hersenen geven een alarmsignaal af zodat de snurker minder diep gaat slapen of (soms benauwd) wakker wordt. |
Volg de multidisciplinaire CBO-richtlijn: OSAS bij kinderen. Bij een vermoeden van een slaapafhankelijke ademhalingsstoornis zoals OSAS dient doorverwezen te worden naar een KNO-arts of kinderarts, of een specialist in een slaapcentrum. |
| Primaire hypersomnieën |
Bij hypersomnie of hypersomnia is er sprake van dagelijks terugkerende perioden van overmatige slaperigheid. Een voorbeeld van een hypersomnie is narcolepsie. Bij narcolepsie is er sprake van oncontroleerbare slaapaanvallen overdag. Ook na voldoende nachtrust. Een zeer zeldzame slaapstoornis is het Kleine-Levin syndroom. Dit syndroom kenmerkt zich door plotselinge zich herhalende episoden van hypersomnie met cognitieve en gedragsstoornissen.[127] |
Bij een vermoeden van een primaire hypersomnie dient verwezen te worden naar een kinderarts of een specialist in een slaapcentrum. |
| Circadiane ritmestoornissen | Bij circadiane ritmestoornissen vindt de aandrijving van het slaap-waakritme door de biologische klok te vroeg of te laat plaats vergeleken met het gewenste ritme. Het endogene vierentwintig uur melatonineritme speelt een sleutelrol bij de synchronisatie van circadiane ritmen, waaronder het slaap-waakritme. Het te vroeg of te laat op gang komen van de endogene melatonineproductie gaat vaak gepaard met stoornissen van het slaap-waakritme. Bij de helft van de kinderen met ADHD is de melatonineproductie gemiddeld één tot anderhalf uur later dan normaal. |
Bij een vermoeden van een circadiane ritmestoornis kan in principe gestart worden met een gedragsmatige aanpak in de JGZ (zie Thema 6: Interventie en begeleiding bij slaapproblemen). Indien deze na een maand nog geen effect heeft, dan doorverwijzen naar een kinderarts of een specialist in een slaapcentrum. Bij hardnekkige circadiane ritmestoornissen en problemen met in slaap vallen kan een behandeling met lichttherapie (zie Thema 6), eventueel aangevuld met melatonine mogelijk effectief zijn. Zie voor de rol van de JGZ professional bij de behandeling met melatonine Bijlage 4. |
| Parasomnieën | Nachtmerries (parasomnia’s) komen voor tijdens de REM slaap, met name tijdens de 2e helft van de nacht. | Bij een vermoeden van parasomniën, kan gestart worden met een interventie in de JGZ (zie Thema 6 Interventie en begeleiding bij slaapproblemen). Indien deze na een maand nog geen effect heeft, dan doorverwijzen naar een kinderarts of een specialist in een slaapcentrum. Raadpleeg de JGZ richtlijn Angst indien er een vermoeden is dat een trauma de oorzaak is van de parasomnie. |
| Nachtelijke verwardheid, slaapwandelen en nachtangst (pavor nocturnus) komen voor tijdens de overgang van diepe naar lichte slaap, met name tijdens de 1e helft van de nacht. | Bij slaapwandelen is het van belang ouders te laten weten dat dit in principe niet gevaarlijk is, maar dat zij wel moeten zorgen dat het kind niet in een onveilige situatie terecht kan komen (bijv. van de trap vallen). | |
| Bij nachtangst (pavor nocturnus) worden kinderen plotseling angstig en overstuur wakker. Het lijkt alsof ze wakker zijn omdat ze hun ogen vaak open hebben, maar dat zijn ze niet. Nachtangst is niet hetzelfde als een nachtmerrie. Het kind kan zich geen nare droom herinneren. Bij een nachtmerrie is dat wel het geval. | Ook bij nachtelijke angst is het belangrijk om ouders gerust te stellen, omdat het er voor ouders uitziet alsof hun kind ergens van overstuur is geraakt. Het kind merkt er echter niets van en kan zich er niets van herinneren. Als ouders het kind tijdens de nachtelijke angst willentroosten, weert het kind hen vaak af en is er nauwelijks contact mogelijk. Hoewel het niet ernstig is en naarmate het kind ouder wordt vanzelf overgaat, kan nachtelijke angst soms worden voorkomen door het kind een kwartier voordat de nachtelijke angst optreed wakker te maken. | |
| Slaapgebonden beweginsstoornissen | Rusteloze benen syndroom, in het Engels “Restless legs syndroom” (RLS): RLS is een neurologische conditie. pijnlijk, brandend of kriebelend gevoel in de benen dat optreedt in rust, met name bij het in slaap vallen, hetgeen problemen met inslapen kan veroorzaken. Er is nog weinig bekend over deze aandoening bij kinderen, maar onderzoek wijst erop dat rond de 2-6% van de kinderen hieraan lijdt. Ook lijkt een ijzertekort te maken te hebben met het ontstaan van RLS. Bij kinderen wordt dit mogelijk nog ondergediagnosticeerd en verward met groeipijnen. Bij chronische groeipijn in combinatie met problemen met inslapen, is het mogelijk dat hier een RLS aan ten grondslag ligt. In 2013 verschenen er op consensus gebaseerde diagnostische criteria door de internationale RLS studiegroep. | Bij een vermoeden van een RLS dient verwezen te worden naar een kinderarts of een specialist in een slaapcentrum. |
| Periodieke bewegingsstoornis van de ledematen, in het Engels “Periodic Limb Movement Disorder” (PLMD): PLMD is een stoornis waarbij kinderen ’s nachts de benen of armen regelmatig, kortdurend en plotseling bewegen, , wat gepaard gaat met kort wakker worden. Kinderen zijn zich niet bewust van het bewegen, maar doordat ze op dat moment ook kort wakker worden, kan het zijn dat ze minder uitgerust raken. Bij periodieke bewegingen van de ledematen ’s nachts, in combinatie met vermoeidheid overdag, kan er sprake zijn van PLMD.[128] Het komt vaak samen met RLS voor. Net als bij RLS lijkt een ijzertekort te maken te hebben met het ontstaan van PLMD. | Bij een vermoeden van een PLMD dient verwezen te worden naar een kinderarts of een specialist in een slaapcentrum. | |
| Tandenknarsen (Bruxisme). De oorzaak is vaak stress gebonden. | Een kind hoeft in principe niet behandeld te worden voor bruxisme, omdat het probleem meestal vanzelf vermindert en niet schadelijk is. Indien het tandenknarsen veelvuldig en langdurig voorkomt kan schade aan de tanden ontstaan. Adviseer ouders in dat geval om een afspraak te maken met een tandarts. Ook kan het tandenknarsen verminderen door spanning bij het kind te verminderen. | |
| Hoofdbonken (Jactatio capitis) komt vaak voor bij jonge kinderen, met name tijdens het inslapen. Het gaat om ritmische, stereotiepe bewegingen in de overgang van waken naar slapen. Het komt bij 20% van de gezonde kinderen voor en het wordt door hen als prettig ervaren. Naast hoofdbonken, kan ook hoofdrollen, “body rolling” of “body rocking” voorkomen, alleen, of in combinatie. Naast het geluid dat de bewegingen veroorzaken, maken veel kinderen ook monotone geluiden bij de bewegingen, die voor veel overlast kunnen zorgen |
Een kind hoeft niet behandeld te worden tegen het hoofdbonken, het gedrag verdwijnt vanzelf weer. Omdat hoofdbonken op ouders beangstigend kan overkomen is het belangrijk gedegen voorlichting te geven. Hoofdbonken kan verergeren door spanningen. Het verminderen van spanning kan ervoor zorgen dat het hoofdbonken afneemt. Hoofdbonken kan verergerd worden als er sprake is van slapeloosheid. Aandacht voor slaaphygiëne is dan belangrijk. Als het kind zichzelf bezeert door het bonken, of het bonken gaat er erg heftig aan toe, kunnen ouders maatregelen treffen om te zorgen dat het kind zich geen pijn kan doen. Bespreek met ouders dat het kindje zich geen pijn doet bij het hoofdbonken. Overleg met ouders wat hierbij met in acht neming van de veilig slapen adviezen de beste oplossingen zijn. Denk bijvoorbeeld aan een campingbedje, waar in het kader van veilig slapen geen matras van een ledikant in gelegd mag worden, maar wel het matras wat hoort bij het campingbedje. Zorg ervoor dat vooral geen koordjes of losliggende kussens worden gebruikt, in verband met het gevaar van verstikking. |
Aanbevelingen
5.1 Zorgen ouders, jeugdige of school
Zorgen van ouders of jeugdigen
De zorgen over slaap van ouders of kinderen zijn vooralsnog leidend. In deze richtlijn wordt bij de definiëring van slaapproblemen uitgegaan van de perceptie van de ouders of de jongere zelf van het slapen, dus van de zorgvraag van de ouders of jongere zelf (zie inleiding voor definitie). Iedere ouder die zorgen heeft over het slapen van het kind, verdient hiervoor adequate aandacht van de JGZ-professional. Dat geldt ook voor kinderen en adolescenten die zelf aangeven problemen te hebben met slapen. Ouders en jongeren kunnen ten einde raad zijn en zelf niet adequaat functioneren door het niet slapen (van hun kind). Tijdens het consult bij de JGZ professional, is er tijd nodig om het verhaal van de ouders en/of het kind zelf goed in kaart te brengen. Empathie maakt interventies effectiever en het bevordert het afstemmen en opvolgen van adviezen. De communicatie tussen professional en ouder(s) en kind(eren) is van groot belang, omdat ouders en kinderen zich door positieve aandacht en bejegening gehoord en begrepen voelen.
Nadat een medische oorzaak van een slaapprobleem is onderzocht, is het in principe niet nodig om een grens te trekken bij een bepaalde hoeveelheid of ernst van het slaapprobleem om voor ondersteuning in aanmerking te komen. Iedere ouder die zorgen heeft over het slapen van zijn kind dient serieus genomen en erkend te worden. Vervolgens wordt eventueel een vragenlijst en een uitgebreide anamnese afgenomen.
Zorgen van (voor)school of het kinderdagverblijf
Slaapproblemen kunnen ook gesignaleerd worden op het kinderdagverblijf en peuterspeelzaal of op school. In de kinderopvang kan het naar bed gaan en inslapen problemen geven en kan een aanleiding zijn voor de pedagogisch medewerker om, na overleg met de ouder, contact op te nemen met de JGZ-medewerker. Bij iets oudere kinderen betreft het veelal het signaleren van problemen met slaperigheid of vermoeidheid overdag, concentratieproblemen en hyperactiviteit die mogelijk het gevolg kunnen zijn van slechte slaap. Ook op het voortgezet onderwijs en MBO kunnen slaapproblemen door docenten worden gesignaleerd. Een enkele keer zullen slaapproblemen op het voortgezet onderwijs en het MBO naar voren komen uit standaard vragenlijsten (o.a. “monitors”) die door de school zelf of de GGD worden afgenomen. Echter, in lang niet alle standaard monitors is een onderdeel over slaap opgenomen. Het is, gezien het belang van slaap voor de gezondheid van kinderen belangrijk, dat het thema “slaap” standaard een plaats krijgt in deze vragenlijsten. Het is belangrijk dat de JGZ samenwerkt met school en het kinderdagverblijf. Dit kan bijvoorbeeld door vertegenwoordiging van de JGZ in de interne zorgstructuur op scholen, zoals een ZAT team of een “bovenschools ondersteuningsteam”.
5.2 Vastellen van oorzaken
De JGZ professional kan oorzaken van slaapproblemen vaststellen door het afnemen van een vragenlijst, een anamnese en het uitvoeren van lichamelijk onderzoek. Zie voor een brede anamnese van slaapproblemen Bijlage 1 Indien ouders of de jongere zelf aangeven dat er sprake is van een slaapprobleem, is het onder meer van belang te vragen naar:
- De slaapduur: slaapt het kind/ de jongere te weinig (perceptie ouders/jongere zelf)?
- Het slaapgedrag: zijn er problemen rond het in slaap vallen? Zijn er problemen met doorslapen?
- Slaperigheid overdag: is het kind/ de jongere overdag slaperig?
- Zijn er ongebruikelijke of vreemde gedragingen ’s nachts (zoals snurken en slaapwandelen).
Belangrijk is dat eerst algemene informatie vergaard wordt in gesprek met de ouders of de jongere zelf. Vervolgens moet een medische oorzaak door een jeugdarts of verpleegkundig specialist worden onderzocht (mogelijk is hiervoor al een vervolgafspraak nodig) en wordt met ouders overlegd of een vervolgafspraak wenselijk is, waarbij door ouders of de jongere zelf een vragenlijst kan worden ingevuld en een brede anamnese wordt afgenomen (zie subsectie Uitgebreide anamnese). Bespreek met ouders of de jongere zelf of zij een slaapdagboek willen bijhouden (zie subsectie Dagboek). Dit geeft meer inzicht in het slaapprobleem voor zowel de JGZ professional als ook voor de ouder of de jongere zelf.
Omdat er in de JGZ geen uitgebreide vragenlijst zal worden ingezet om slaapstoornissen te diagnosticeren en te onderscheiden van slaapproblemen, is het mogelijk dat kinderen met een slaapstoornis gemist worden. De werkgroep acht het risico op ernstige gevolgen hiervan echter klein. Bij ernstige aandoeningen die met slaap te maken hebben, zullen in de meeste gevallen ook andere problemen spelen die aandacht van de JGZ professional zullen trekken. Niet tijdig ingrijpen van de JGZ professional bij een slaapstoornis zal hooguit een vertraging opleveren van doorverwijzing en adequate behandeling (zie sectie Begeleiden en behandelen en sectie Samenwerken en verwijzen), wat naar mening van de werkgroep geen ernstige gevolgen zal opleveren voor de gezondheid van het kind. Wel is het belangrijk ouders adequaat te ondersteunen als zij aangeven dat er sprake is van een slaapprobleem. Ook kunnen ouders in een crisissituatie zijn beland. Zij moeten uiteraard adequaat geholpen worden, omdat in dat geval de veiligheid van het kind mogelijk gevaar loopt. De vraag ‘Kun je de situatie nog aan?’ of ‘Zie je de komende nacht nog zitten?’ is dan opportuun. Het borgen van de veiligheid van het kind is essentieel (zie de sectie Behandelen en begeleiden).
Lichamelijk onderzoek
Een medische oorzaak voor het slaapprobleem moet worden onderzocht door een jeugdarts of verpleegkundig specialist, voor zover mogelijk. Veel medische oorzaken en slaapstoornissen, zoals het obstructieve slaap-apneu syndroom, kunnen door een jeugdarts of verpleegkundig specialist echter nooit volledig worden uitgesloten, omdat hiervoor een slaaponderzoek met nachtelijke opname nodig is. In het overzicht hieronder worden enkele voorbeelden gegeven van medische aandoeningen die slaapproblemen kunnen veroorzaken (zie Tabel 1). Indien er op basis van het lichamelijk onderzoek een vermoeden is van een medische oorzaak, wordt een inschatting gemaakt of JGZ alsnog adequaat kan interveniëren. Indien dit niet het geval is, of indien de ingezette interventie na een maand nog geen effect heeft, wordt het kind rechtstreeks verwezen naar een kinderarts of een specialist in een slaapcentrum (zie Thema 7).
Pathologie behorende bij slaapstoornissen of slaapproblemen is medisch gezien niet schadelijk wanneer het in een enkel geval niet direct onderkend wordt. Wanneer er een kans of verdenking is van mishandeling, is altijd spoed noodzakelijk (zie JGZ-richtlijn Kindermishandeling).
Daarnaast is het mogelijk dat kinderen medicijnen gebruiken die de slaap beïnvloeden. Zie voor uitgebreide informatie over de relatie tussen geneesmiddelen en slaap (zie de subsectie Melatonine en andere geneesmiddelen).
Bij het lichamelijk onderzoek is het belangrijk te letten op:
- Vergrote amandelen
- Rhinitis
- Otitis Media
- Moeilijke ademhaling, benauwdheid
- Atopie, eczeem of andere huidaandoeningen
- Mondgezondheid
Tabel 1. Veel voorkomende medische aandoeningen die een slaapprobleem kunnen veroorzaken.
| Aandoeningen/pathologie | Presentatie als slaapprobleem | Te ondernemen actie |
| Gastro-oesofageale reflux (ziekte)(GER) |
Gastro-oesofageale reflux is het terugvloeien van de maaginhoud in de slokdarm. Bij baby’s is de sluitspier tussen de maag en de slokdarm nog niet volledig ontwikkeld. Daardoor kan er (zure) maaginhoud terugvloeien in de slokdarm. Dit gebeurt vooral in horizontale positie, zoals tijdens de slaap. Gastro-oesofageale refluxziekte (GORZ) treedt op als de reflux van maaginhoud leidt tot hinderlijke klachten en/of complicaties zoals overmatig huilen, prikkelbaarheid, voedselweigering en groeivertraging bij jongere kinderen. |
Verwijs bij slaapproblemen die te maken hebben met reflux door naar de huisarts of kinderarts. In de NVK richtlijn Gastro-oesofageale reflux(ziekte) staat dat: Bij zuigelingen (kinderen ≤18 maanden) met klachten van reflux wordt, net als bij andere zuigelingen, rugligging tijdens het slapen geadviseerd (i.v.m. preventie wiegendood). Verder is, afhankelijk van de ernst van de klachten, linker zijligging in bed een behandeladvies bij oudere kinderen (> 18 maanden). Bij adolescenten wordt daarnaast het verhogen van het hoofdeinde geadviseerd. |
| Verstopte neus | Verstopte neus en adembelemmering kunnen slaap verstoren | Dit slaapprobleem lost in de meeste gevallen vanzelf weer op, als de verstopte neus verholpen is. Stel ouders gerust dat het slaapprobleem waarschijnlijk van tijdelijke aard is en vanzelf weer over gaat. Als dat niet het geval is, adviseer contact op te nemen met de huisarts. |
| ’s nachts hoesten |
Kinderen met symptomen van astma kunnen zich moe en uitgeput voelen door gebrek aan slaap ten gevolge van aanvallen van benauwdheid en nachtelijk hoesten. |
Volg JGZ-richtlijn Astma bij kinderen |
| Jeuk, atopie, eczeem, allergieën, en andere huidaandoeningen | Kinderen (ongeacht de leeftijd) met jeuk, al dan niet door eczeem hebben vaak meer moeite om in slaap te vallen, worden ’s nachts vaker wakker, slapen vaak en voelen zich overdag vermoeid. |
Volg JGZ-richtlijn Huidafwijkingen In de JGZ-richtlijn Huidafwijkingen wordt aanbevolen om de slaapproblemen die ontstaan door jeuk en eczeem te behandelen binnen de JGZ. Adviseer ouders om bij jeuk en eczeem een consequente bedtijd te blijven hanteren. Ook bij kinderen met jeuk of eczeem kan een gedragsmatige slaapinterventie ouders ondersteunen bij het beter laten slapen van hun kind: Specifiek bij baby’s: Het is voor ouder en kind prettig als het kind ondanks de jeuk/eczeem toch leert om ’s nachts door te slapen. |
| Pijn |
Bij kinderen met (chronische) pijn komen vaker slaapproblemen voor dan bij gezonde kinderen. Denk hierbij bijvoorbeeld aan oorpijn. Bij groeipijn kan mogelijk sprake zijn van Restless legs syndroom (RLS) (zie Tabel 2) |
Zie ook de behandeling van slaapproblemen bij jeuk, atopie, eczeem, allergieën, en andere huidaandoeningen |
| Onvoldoende ijzer | Onvoldoende ijzer kan bloedarmoede veroorzaken en in sommige gevallen kan dit zorgen voor vermoeidheid overdag. Een ijzertekort lijkt daarnaast te maken te hebben met het ontstaan van het rusteloze benen syndroom en de periodieke bewegingsstoornis van de ledematen (zie tabel 2 van dit hoofdstuk). | Volg JGZ-richtlijn Voeding en eetgedrag |
| Overgewicht | Verschillende studies laten een verband zien tussen een slaaptekort en overgewicht. |
Overgewicht geeft kans op slaapapneu (zie tabel 2) en daardoor klachten overdag. Deze klachten kunnen bij kinderen met overgewicht sterk variëren en is ook afhankelijk van de leeftijd. Sommige kinderen worden moe en slaperig (dit geldt meestal voor de wat oudere obese kinderen) andere kinderen kunnen juist hyperactief worden. Omgekeerd kan te weinig slapen mogelijk mede oorzaak zijn van het ontstaan van obesitas. Volg de JGZ-richtlijn Overgewicht. Bespreek met ouders of zij van mening zijn dat het kind (te) kort slaapt, ook al is hij/zij niet vermoeid overdag en leg uit dat kinderen met overgewicht soms onvoldoende slapen, terwijl dit niet altijd hoeft te resulteren in vermoeidheid overdag. Laat ouders/jongere een slaapdagboek invullen (zie subsectie Dagboek) . Overweeg ouders/jongeren voor te lichten over het belang van een gezonde slaap en slaaphygiëne (zie sectie Preventie of een interventie voor een slaapprobleem (zie Sectie Begeleiden en behandelen) indien de jeugdige ‘s nachts kort slaapt. |
5.3 Uitgebreide anamnese bij slaapproblemen van kinderen en jongeren
Deze uitgebreide anamnese is gebaseerd op de methodiek van Schregardus en de brede anamnese voor psychosociale problematiek uit de (concept) JGZ richtlijn Depressie. Het is bedoeld om een goed beeld te krijgen van de situatie en het ontstaan van mogelijk foutieve patronen bij het in- en doorslapen. Bij het onderzoek moet rekening gehouden worden met de mogelijk hoge intra-individualiteit. Dit betekent dat het gedrag bij hetzelfde kind niet constant hoeft te zijn. Slaapproblematiek is gedrag met een redelijk hoge intra-individualiteit.
Om goede begeleiding en hulp te kunnen geven is het voor zowel professional als cliënt belangrijk om eerst een goed beeld te krijgen van het slaapprobleem (de probleemverheldering). Vervolgens is het belangrijk dat de factoren in kaart gebracht worden die het slaapprobleem veroorzaken of in stand houden (de probleemanalyse). Ook is het goed om te weten wat er al is geprobeerd om het probleem op te lossen, wat werkt en niet werkt.
Bij een groot slaapprobleem (crisissituatie of complexe problematiek) is het aan te raden om een meer uitgebreide anamnese af te nemen. Het is belangrijk altijd je vragen in te leiden; vertel aan de ouders of de jongere waarom je de(ze) vragen gaat stellen.
Hanteer de hier opgestelde vragen als leidraad, en pas ze aan de situatie en de leeftijd van het kind aan. Ga bij onderstaande vragen uit van je eigen deskundigheid. Bij weinig ernst of trauma’s kun je vragen als volgt samenvatten: “Waren er dingen ingrijpend in het leven van uw kind, bijv. tijdens de zwangerschap of geboorte, de ontwikkeling, was het kind gewenst, etc?”
De anamnese bestaat uit veel gerichte en gesloten vragen. Nodig de ouders en jongeren uit om zoveel mogelijk kort te antwoorden (en uitvoeriger waar nodig).
Daarnaast is het een vereiste om ieder gezin als uniek te benaderen door:
- De informatie met veel aandacht en genuanceerd in te winnen
- Vragend te blijven, nooit stellend te worden
- De ouders of de jongere de keus te laten
5.3.1 Anamnese bij jonge kinderen
Probleemverheldering
Als ouders het slaapprobleem geen ‘probleem’ noemen, zou je kunnen spreken van ‘slaappatroon’.
- Kun je meer vertellen over het slaapprobleem?
- Wanneer zijn de slaapproblemen begonnen?
- Was er een speciale aanleiding voor het ontstaan van het slaapprobleem in de tijd?
- Hoe heeft het slaapprobleem/patroon zich ontwikkeld daarna?
- Hoe lang duurt het slaapprobleem al?
- Gebeurt het elke nacht? Op welk moment?
- Wat zijn de gevolgen?
- Wat zou je graag veranderd willen zien?
- Wat vinden jullie het meest vervelend of waar maken jullie je de meeste zorgen over?
Gedrag ouders
- Wie brengt het kind naar bed? Wanneer? Hoe gaat dat?
- Wat gebeurt er als je weg wilt gaan?
- Hoe gaat het verder de avond en nacht? Wie gaat er naar het kind toe?
- Hoe reageren jullie op het kind? Reageren jullie hetzelfde?
- Wat roept het gedrag van het kind ’s avonds/’s nachts bij jullie zelf op: onmacht/angst/boosheid/bezorgdheid/etc.?
- Op welke manier tanken jullie zelf bij? Waar halen jullie je energie vandaan?
Slaaphygiëne
- Waar slaapt het kind? Waar valt het kind in slaap?
- Slaapt het kind alleen in een kamer, of bij ouders of met broertjes of zusjes?
- Valt het kind meteen in slaap of ligt het lang wakker? Hoe lang denk je gemiddeld? Wat doe je dan?
- Tijdstip van naar bed gaan (is dit elke nacht ongeveer hetzelfde, verschil doordeweeks/weekend)
- Slaapt het kind overdag?
- Slaapt het kind in een donkere kamer, of is er veel licht?
- Is de temperatuur goed in de kamer?
- Geef je het kind iets te eten of te drinken voor het slapen gaan?
- Wat doet het kind ’s avonds, vlak voor het slapen gaan (denk aan Tv-kijken, computeren, wilde spelletjes etc.)
- Gebruikt het kind medicatie? (Raadpleeg ook het JGZ dossier)
- Gebruikt het kind cafeïne of genotmiddelen? (denk aan cola, koffie, energiedrankjes, sigaretten, alcohol, drugs, etc.)
- Snurkt het kind?
- Slaapwandelt het kind? Ander opvallend gedrag ’s nachts?
- Heeft het kind nachtmerries?
Probleemanalyse voorgeschiedenis
Afhankelijk van de problematiek kunnen de volgende vragen wat uitgebreider of juist kort doorlopen worden
- Was het kind gewenst?
- Hebben jullie lang uitgekeken naar de zwangerschap?
- Zwangerschap goed verlopen?
- Bevalling zonder complicaties?
- Hoe was de start van het kind?
- Is het kind lichamelijk gezond geweest tot nu toe?
- Zijn er bijzonderheden t.a.v. de voeding geweest (borst/fles)?
- Hoe was de motorische ontwikkeling? Bijv. rollen – zitten – kruipen – staan – wanneer liep het kind los?
- Hoe ervaren de ouders het kind, wat voor een type kind vinden zij het?
- Wie zorgde/zorgt voor het kind overdag – ’s avonds – weekend?
- Is er ook nog een andere soort opvang? Hoe gaat dat?
- Hoe is het met de zindelijkheid dag – nacht (gegaan)?
- Zijn er ingrijpende gebeurtenissen geweest in het leven van het kind tot nu toe, die van invloed kunnen zijn op het huidige gedrag?
Huidige situatie (algemeen)
Afhankelijk van de problematiek kunnen de volgende vragen wat uitgebreider of juist kort doorlopen worden
- Zijn er ook problemen overdag?
- Is er – om wat voor reden dan ook – spanning bij jullie in huis?
- Hoe gaat het samen met het (de) andere kind(eren)?
- Wat voor effect heeft de huidige situatie op jullie en de andere gezinsleden.
- Soms hangt het gedrag van kinderen sterk samen met een fase in de ontwikkeling. Denkt u dat het gedrag van uw kind kan samenhangen met de leeftijdsfase waarin uw kind verkeert?
- Kan het kind zichzelf goed vermaken?
- Heeft het kind/gezin een vaste dagindeling?
- Hoe ziet dat eruit?
- Wat zijn de leuke kanten van dit kind? m.a.w. Wat gaat goed? Waar genieten jullie van?
- Hebben jullie dezelfde ideeën over opvoeden?
- Reageren jullie hetzelfde op het kind?
- Wat doet het kind als het z’n zin niet krijgt?
- Hoe reageren jullie op het gedrag van het kind als het z’n zin niet krijgt? Hoe gaat het verder? Hoe loopt het af?
- Hoe maken jullie het verschil tussen ja en nee duidelijk?
- Weet het kind het verschil tussen ja en nee? Hoe merk je dat?
Sociaal netwerk
- Krijg je hulp of steun van familie of vrienden?
- Heb je om hulp gevraagd aan anderen?
- Aan wie (sociaal netwerk en/of professional)?
- Heb je hulp gekregen?
- Zo ja van wie, en wat heeft het je opgeleverd?
Eerdere oplossingen
- Wat hebben jullie tot nu toe geprobeerd om de slaapproblemen op te lossen of het patroon te veranderen? Wat werkt er wel?
- Waarom lukt het niet de problemen op te lossen of patronen te veranderen?
- Heb je informatie opgezocht?
- Welke informatie heb je gevonden?
- Had je daar wat aan; zo ja, wat?
- Heb je dingen uitgeprobeerd om het probleem op te lossen?
- Wat was het effect; ben je daar tevreden over?
- Zo nee, heb je ideeën over wat mogelijk nog wel zou kunnen werken?
- Zijn er al dingen veranderd?
Vervolg
- Noodzaak voor een vervolg (eventueel schaalvraag)
- Zou je hulp willen en zo ja van wie en hoe?
Samenvatting
Conclusie
Gezamenlijke afspraken over het vervolg
5.3.2 Anamnese oudere kinderen/jongeren
Vragen die bruikbaar kunnen zijn bij een uitgebreide brede anamnese.
Probleemverheldering
- Wat is het ervaren probleem?
- “Kun je er meer over vertellen?”
- Wat gebeurt er?
- Op welke momenten?
- Hoe vaak?
- Hoeveel last heb je ervan (schaalvraag eventueel)?
- Wat zijn de gevolgen? Wat merk je ervan?
Aanleiding
- Sinds wanneer is het?
- Was er een aanleiding; weet je waarom je slecht bent gaan slapen?
- Zou het ergens mee te maken kunnen hebben denk je?
Slaaphygiëne
- Waar slaap je/ waar val je in slaap?
- Tijdstip van naar bed gaan (is dit elke nacht ongeveer hetzelfde, verschil doordeweeks/weekend)
- Val je meteen in slaap of lig je lang wakker? Hoe lang denk je gemiddeld? Wat doe je dan?
- Word je ’s nachts wakker en wat doe je dan?
- Slaap je overdag weleens?
- Slaap je alleen in een kamer?
- Slaap je in een donkere kamer, of is er veel licht?
- Is de temperatuur goed in de kamer? Niet te warm, en niet te koud?
- Eet je iets, voordat je naar bed gaat?
- Wat doe je ’s avonds, vlak voor het slapen gaan (denk aan Tv-kijken, computeren , etc.)
- Gebruik je het bed voor andere activiteiten dan slapen? Bijv. studeren, telefoneren, gamen etc.)
- Gebruik je medicatie? (Raadpleeg ook het JGZ dossier)
- Gebruik cafeïne en genotmiddelen? (denk aan cola, koffie, energiedrankjes, sigaretten, alcohol, drugs, etc.)
- Snurk je?
- Slaapwandel je weleens, of heb je last van ander opvallend gedrag ’s nachts?
- Heb je nachtmerries
Gezinssituatie
- Hoe ziet jullie gezin eruit (bij wie woon je)?
- Hoe gaat het thuis met de verschillende gezinsleden?
- Relatie met verschillende gezinsleden?
- Zijn er de afgelopen twee jaar ingrijpende gebeurtenissen geweest in jullie gezin?
School
- Hoe gaat het op school?
- Wat vind je van school?
- Wat vind je leuk om te doen?
- Wat vind je minder leuk aan school?
- Hoe zijn je resultaten?
- Concentratie / aandacht?
- Wie zijn je vrienden?
- Wordt er gepest op school / in de klas?
- Wordt je wel eens gepest, of pest je zelf?
Vrije tijd
- Wat vind je leuk om te doen?
- Heb je vaste bezigheden?
- Hoeveel tijd besteed je er aan?
- Spreek je af met vrienden?
Stemming
- Hoe is je stemming in het algemeen (vrolijk, ongelukkig, verdrietig);
- Is er sprake van angst, zenuwachtigheid of gepieker;
- Is er iets veranderd daarin de laatste tijd?
Sociaal netwerk
- Heb je om hulp gevraagd aan anderen?
- Aan wie (sociaal netwerk en/of professional)?
- Heb je hulp gekregen?
- Zo ja van wie, en wat heeft het je opgeleverd?
Eerdere oplossingen
- Wat heb je zelf al geprobeerd om het probleem op te lossen?
- Heb je informatie opgezocht;
- Welke informatie heb je gevonden;
- Had je daar wat aan; zo ja, wat;
- Heb je dingen uitgeprobeerd om het probleem op te lossen;
- Wat was het effect; ben je daar tevreden over;
- Zo nee, heb je ideeën over wat mogelijk nog wel zou kunnen werken?
- Zijn er al dingen veranderd?
Vervolg
- Noodzaak voor een vervolg (eventueel schaalvraag)
- Zou je hulp willen en zo ja van wie en hoe?
Samenvatting
Conclusie
Gezamenlijke afspraken over het vervolg
Bron
- Zorgplan JGZ (2008 V&VN)
- JGZ Richtlijneno.a.
- Opvoedingsondersteuning kaart 2 “beslisschema”
- Vroegsignalering van psychosociale problemen Balansmodel (tabel 2.1)
- Depressie (concept)
- Angst
5.4 Gevalideerde Nederlandse vragenlijsten
Indien de JGZ professional ouders of de jongere zelf daartoe in staat acht, ouders of de jongere zelf vragen om een vragenlijst in te vullen, voorafgaand aan het volgende contactmoment. Deze vragenlijsten kunnen een deel van de brede anamnese in de subsectie Uitgebreide anamnese vervangen.
In deze bijlage zijn de volgende vragenlijsten opgenomen:
- De “ Slaapgewoonten Vragenlijst” (Child Sleep Hygiene Questionnaire, CSHQ).[125] Deze vragenlijst bestaat uit 33 vragen over slaapgewoonten en is gevalideerd voor ouders van kinderen van 4-10 jaar.
- De “Slaaphygiëne Vragenlijst” (Adolescent Sleep Hygiene Scale, ASHQ).[47] Deze vragenlijst werd in Nederland onderzocht en gevalideerd voor adolescenten. Deze vragenlijst bestaat uit 28 items over slaaphygiëne.
- De “Chronisch Slaaptekort Vragenlijst” (Chronic Sleep Reduction Questionnaire, CSRQ).[126] Deze vragenlijst werd eveneens onderzocht en gevalideerd voor Nederlandse adolescenten. De vragenlijst bestaat uit 20 items over slaaptekorten.
5.4.1 De slaapgewoonten Vragenlijst (CSHQ)
De slaapgewoonten vragenlijst bestaat uit 33 vragen over slaapgewoonten en is gevalideerd voor ouders van kinderen van 4-10 jaar.
Waumans RC, Terwee CB, Van den Berg G, Knol DL, Van Litsenburg RR, Gemke RJ. Sleep and sleep disturbance in children: Reliability and validity of the dutch version of the child sleep habits questionnaire. Sleep. 2010;33(6):841-845.
van Litsenburg RR, Waumans RC, van den Berg G, Gemke RJ. Sleep habits and sleep disturbances in Dutch children: a population-based study. Eur J Pediatr. 2010 Aug;169(8):1009-15.
5.4.2 Slaaphygiëne vragenlijst (ASHQ)
De Slaaphygiëne Vragenlijst voor adolescenten wordt op een 6 puntsschaal gescoord. Een hogere score duidt op een betere slaaphygiëne. Deze versie van de vragenlijst is gebruikt in het onderzoek van Tamar van Kooten en is gebaseerd op de vragenlijst van LeBourgois et al.[169]
5.4.3 Chronisch slaaptekort Vragenlijst (CSRQ)
De Chronisch Slaaptekort Vragenlijst beoogt chronisch slaaptekort te meten in kinderen en adolescenten. De vragenlijst staat gedetailleerd beschreven in het artikel van Meijer et al.[170]
De Chronisch Slaaptekort Vragenlijst bestaat uit 20 vragen en wordt op een 3 puntsschaal gescoord, hoe hoger de score hoe meer chronisch slaaptekort een individu heeft. Wanneer antwoord 1 is aangekruist, wordt een score van 1 gegeven, antwoord 2 = 2, antwoord 3 = 3. Vragen 2, 5, 11 en17 moeten gehercodeerd worden. Dit betekent dat dan antwoord 1 de score 3 krijgt en antwoord 3 de score 1. Antwoord 2 behoudt de score 2.
Optelling van alle scores geeft een indicatie voor een algemene mate van chronisch slaaptekort. De minimum score voor de totale schaal is 20 en de maximum score 60. De schaal bestaat uit 4 verschillende subschalen: Slaaptekort (vraag 1, 5, 6, 7, 17, 18), irritatie (vraag 9, 10, 14, 19, 20 ), energie verlies (vraag 2, 11, 12, 15, 16) en slaperigheid (vraag 3, 4, 8, 13 ).
Als afkappunt voor chronisch slaaptekort wordt een score van 40 gehanteerd. Deze score is gelijk aan 1 standaarddeviatie boven het gemiddelde.[126][171][172]
Informatie over de relaties van de Chronisch Slaaptekort Vragenlijst met functioneren overdag is te vinden in Dewald-Kaufmann, et al.[173]
5.5 Dagboek
Indien er na gedegen anamnese, lichamelijk en psychosociaal onderzoek geen aanwijzingen zijn voor onderliggende pathologie, kan worden gestart met het invullen van een gevalideerd 24-uurs dagboek. Het bijhouden van een dagboek kan ouders en jeugdigen meer inzicht geven in het slaapprobleem en of er verbeteringen optreden. Een enkele meting is niet voldoende, het minimum is 3 dagen en nachten (herhaalde metingen). Hierbij kan gebruik worden gemaakt van het gevalideerde 24-uurs dagboek van Barr.[174] Dit is gevalideerd aan de hand van geluidsopnamen en actigrafie, zowel voor de papieren versie als de elektronische versies. [175][176] Voor baby’s is het dagboek beschikbaar via de JGZ richtlijn excessief huilen. Bij slaapproblematiek kan ouders worden gevraagd op een aaneengesloten periode van dagen een 24-uurs dagboek in te vullen, om inzicht te krijgen in duur, frequentie en perioden van slaap, wakker zijn, huilen, gevoed en verzorgd worden en waar de baby zich bevindt. Het bijhouden van een 24-uurs dagboek, met zowel de activiteiten van de baby als de reacties van de ouders, is een hulpmiddel om ouders en zorgverlener inzicht te geven in de mate en de ernst van het slaapprobleem. Ernst, frequentie, duur en ouderperceptie van slaap kan ook voor oudere kinderen worden bepaald met behulp van zo’n 24-uurs dagboek. Bij het gebruiken van een dagboek naar slaap dient altijd de volgende kanttekening te worden gemaakt; ouders weten nooit zeker of een kind wakker is of slaapt. Het kind kan ook wakker, maar stil in bed liggen.
Ook voor oudere kinderen en adolescenten zijn slaapdagboeken gevalideerd. Meestal worden deze voor de duur van 1 week ingevuld. Bij volwassenen is er consensus over wat er in een slaapdagboek moet worden bijgehouden, maar bij kinderen is dat er niet.[177] Bij slaapdagboeken bij kinderen en adolescenten worden meestal de totale slaapduur, de tijd van naar bed gaan, van het in slaap vallen, de tijd van opstaan, het aantal keren wakker worden, de duur van het ’s nachts wakker liggen en vaak ook of het kind overdag slaapt bijgehouden.[176][178][179] Het is belangrijk om gedrag 24 uur, meerdere dagen achter elkaar te meten, zodat je veranderingen en verschuivingen op kan merken in, en het dagboek niet incidenteel in laat vullen. Hieronder volgen verschillende voorbeelden van dagboeken voor kinderen van verschillende leeftijden.
Op internet zijn verschillende voorbeelden van dagboeken te vinden. Deze zijn ontwikkeld voor volwassenen, maar kunnen ook door adolescenten worden gebruikt. Bijvoorbeeld: https://www.nhg.org/sites/default/files/content/nhg_org/uploads/standaard/download/slaapdagboek.pdf of https://www.thuisarts.nl/sites/default/files/slaapdagboek.pdf
In de toekomst zijn mogelijke alternatieven voor het dagboek apps of gadgets die slaap meten d.m.v. sensoren, zoals: Fitbit, Jawbone UP, SleepTracker, Lark, Melon, Sleep Cycle, Sleep Bot, Sleep as Android en de Mimo baby monitor. Er is echter nog geen onderzoek gedaan naar de validiteit van deze “gadgets” voor wat betreft het signaleren van slaapproblemen.
Slaapdagboek 0-4 jaar: zie Bestanden
Slaapdagboekje, kinderen van 6 maanden tot 4 jaar:
Slaapdagboek voor kind/jongere (6-18 jaar): zie Bestanden
6 Begeleiden en behandelen
In deze sectie wordt ingegaan op verschillende behandelingen bij slaapproblemen die door de JGZ kunnen worden toegepast.
Veel slaapproblemen kunnen worden voorkomen (zie de sectie Preventie.)
Als slaapproblemen ontstaan is er een grote kans dat zij vanzelf over gaan. Er zijn echter ook effectieve behandelingen voor slaapproblemen die door de JGZ kunnen worden ingezet. Daarnaast zijn er effectieve behandelingen voor slaapproblemen en slaapstoornissen buiten de JGZ (zie de sectie Samenwerken en doorverwijzen).
Veiligheid
Bij slaapproblemen ontstaan regelmatig crisissituaties, waarbij de vraag of ouders in staat zijn de situatie te hanteren centraal moet staan. De werkgroep stelt voor dat de vraag ‘Kun je de situatie nog aan?’ of ‘Zie je de komende nacht nog zitten?’ altijd gesteld moet worden (feitelijk moet deze vraag bij de start van iedere interventie gesteld worden). Het borgen van de veiligheid van het kind is essentieel. Is dit niet te garanderen, dan wordt in eerste instantie het sociaal netwerk aangesproken. Is dit niet voor handen, dan is een ziekenhuisopname op sociale indicatie gepast.
Aanbevelingen
6.1 Effectieve interventies
6.1.1 Tot 6 maanden
Op de leeftijd voor 6 maanden is, als er sprake is van een slaapprobleem, in de meeste gevallen ook sprake van een probleem met (excessief) huilen. Volg hiervoor de Multidisciplinaire richtlijn Excessief huilen. In deze richtlijn komt o.a. het effect van adviezen van regelmaat en voorspelbaarheid, al dan niet in combinatie met inbakeren ter sprake. Inbakeren was vroeger een gewoonte en wordt ook nu nog vanuit traditie in het Midden Oosten regelmatig toegepast. In Westerse landen wordt inbakeren in combinatie met adviezen van regelmaat en voorspelbaarheid regelmatig ingezet als tijdelijke interventie bij excessief huilen (zie ook de Multidisciplinaire Richtlijn Excessief huilen). Ingebakerde kinderen worden minder vaak wakker, slapen langer en hebben een verhoogde zelfregulatie. Het algemeen geldend advies in Nederland is dat inbakeren niet direct vanaf de geboorte ingezet wordt, maar alleen als er sprake is van excessief huilen en wanneer de adviezen van regelmaat en voorspelbaarheid onvoldoende effect sorteren.[153] Uit onderzoek blijkt dat bij excessief huilende baby’s de slaap binnen een week toenam bij zowel rust, regelmaat en voorspelbaarheid met en zonder inbakeren. Van groot belang is dat het inbakeren gestaakt wordt zodra het kind begint met pogingen tot omrollen.
5 S’en methode/ The Happiest Baby
Dr. Harvey Karp ontwikkelde de 5 S’en methode in zijn boek “The Happiest Baby on the Block”. Deze methode houdt kortweg in dat ouders vijf technieken toepassen die ervoor zouden moeten zorgen dat een baby binnen korte tijd stopt met huilen. De vijf technieken, die in het engels allen met een “S” beginnen zijn:
- Inbakeren (Swaddling),
- Houd de baby op de zij/buik gedraaid op je arm (Side/Stomach position),
- Sus de baby met “shhh” (Shushing),
- Wieg de baby (Swinging),
- Geef de baby iets om op te zuigen (speen) (Sucking).
Er werden tot nu toe twee onderzoeken gedaan naar deze techniek, waarvan in één artikel werd gekeken naar het effect op de slaap van baby’s. In een RCT kregen 35 ouders van pasgeboren baby’s in de interventiegroep een video te zien waarin de methode werd getoond.[134] In de controlegroep kregen ouders standaard advies via een video. Na de interventie was er geen significant verschil tussen de interventie en de controlegroep wat betreft het huilen en slapen gedurende de eerste, vierde, zesde, achtste en twaalfde week van het leven van de baby. In de twaalfde week hadden ouders in de interventiegroep meer stress dan ouders in de controlegroep. In een reactie op dit artikel stelt dr. Harvey Karp dat dit onderzoek nog geen bewijs is dat zijn methode niet werkt, omdat niet duidelijk is of ouders de video daadwerkelijk bekeken hadden.[164] Daarnaast stelt hij dat ouders niet inbakerden, zoals gedemonstreerd in de video.
Het enige andere onderzoek naar de methode, toegepast door een onderzoeker, had geen slaap als uitkomstmaat.[165] In dat onderzoek werden significante verschillen tussen de 5s’en en controlegroepen gerapporteerd wat betreft pijnscores en duur van het huilen na een vaccinatie. De groepen waarbij de 5s’en werd toegepast hadden de laagste pijnscores en huilduur.
Massagetherapie
Er zijn enkele aanwijzingen dat massagetherapie een positief effect heeft op de slaap van baby’s en jonge kinderen met autisme. [131][132][133]
6.1.2 Jonge kinderen (vanaf 6 maanden)
Uitdoven
De meeste hieronder beschreven gedragsmatige interventies bij jonge kinderen zijn gebaseerd op het laten uitdoven van ongewenst gedrag (extinctie), waaronder huilen, aandringen en roepen om de ouders. Uitdoving in ongemodificeerde (pure) vorm staat ook wel bekend als ‘laten huilen’. Begrijpelijkerwijs roept deze term weerstand op, omdat dit de suggestie wekt dat de baby aan zijn lot wordt overgelaten. In Nederland staat deze methode bekend als o.a. de methode Schregardus.[157] In deze methode is het negeren van het huilen van de baby slechts een onderdeel. De methode kent zowel overdag als ’s nachts meer elementen, zoals het leren onderscheiden van verschillende soorten huilen, met consequenties voor wel of niet reageren. Er zijn, zoals hieronder beschreven, allerlei modificaties ontwikkeld voor uitdoving, die het negeren van het huilen aanzienlijk reduceren. Evenals voor de ongemodificeerde vorm, bestaat wetenschappelijk bewijs voor het positieve effect van deze methoden op het slaapprobleem op korte en middellange termijn. Toch roepen al deze methoden, gemodificeerd of niet, de vraag op of een kind schade ondervindt, wanneer het een appel doet op de ouder, waarop het niet direct een respons ervaart. Om deze reden is Bijlage 7. toegevoegd aan de richtlijn. Hierin wordt uiteengezet wat de huidige wetenschappelijk inzichten zijn rondom uitdoving, sensitief en responsief opvoeden bij een kind wat niet slaapt.
Er is geen bewijs dat gedragsinterventies bij slaapproblemen schadelijk zijn.[158] Onderstaande interventies zijn, mits correct uitgevoerd en goed begeleid, in principe veilig en effectief.[159][160][161][162] Uiteraard moet bij het uitvoeren van deze interventies rekening worden gehouden met de wensen van ouders. Wanneer ouders het niet wenselijk vinden om hun kind enige tijd alleen te laten huilen, zoals bij ongemodificeerde uitdoving, staan voor hen aangepaste versies ter beschikking, zoals uitdoving met aanwezigheid van de ouders en graduele uitdoving.
Ongemodificeerde uitdoving
Een interventie voor in- en doorslaapproblemen waar veel onderzoek naar is gedaan, wordt uitdoving of “extinctie” genoemd. De interventie staat bij veel ouders bekend als de “laten huilen” techniek. In principe bestaat deze interventie uit het in bed leggen van het kind op een door ouders gewenste tijd, waarna ouders het kind op een door ouders gewenste tijd van opstaan weer uit bed halen. Als het kindje tijdens de nacht huilt, of het de ouders roept of boos wordt, moeten ouders niet naar het kind toe reageren. Ouders blijven wel altijd controleren op ziekte of verwondingen bij het kind.[20][130]
De interventie is gebaseerd op de leertheorie, waarin verondersteld wordt dat de aandacht die ouders geven als het kind wakker is, voor het kind heeft gewerkt als beloning. Hierdoor wordt het slaapprobleem in stand gehouden. Uitdoving van het slaapprobleem zou dan kunnen worden bereikt om de “beloning” (aandacht van de ouder) weg te nemen.[2]
De interventie wordt toegepast in combinatie met de tips voor slaaphygiëne, zoals het doorlopen van een vaste routine bij het naar bed gaan en vaste bedtijden. Vooraf wordt het kind altijd verteld dat de ouder niet zal komen als het kind roept of schreeuwt. Het moet precies weten waar het aan toe is en de ouder moet van de JGZ professional duidelijk toelichting krijgen hoe ze dat helder en duidelijk kunnen overbrengen aan het kind. Ouders wordt ook verteld dat er terugvalmomenten kunnen voorkomen. Dan komt op een later moment het eerdere problematische gedrag weer terug. Aan ouders wordt uitgelegd om de draad weer op te pakken, zoals ze gestart zijn met de aanpak en het problematische gedrag volgend op zo’n terugval niet te versterken.
Onderzoek toont aan dat de methode effectief is. Na drie dagen is het slaapprobleem in de meeste gevallen over. Er zijn echter ook nadelen aan het toepassen van deze techniek. Ouders kunnen het erg moeilijk vinden om hun kind te laten huilen en gaan soms toch reageren. Het kind zal dan leren dat het de volgende keer weer zo lang moet huilen en dat de ouders dan toch komen. De interventie vergt veel doorzettingsvermogen van ouders.
We adviseren professionals om met ouders af te spreken om meteen na de eerste nacht contact op te nemen om te vragen hoe de nacht is verlopen. Als er in de loop van drie dagen geen verandering is, is het belangrijk om samen met ouders te bespreken hoe zij het toepassen van de interventie hebben ervaren en om te kijken of zij de interventie zoals bedoeld willen en kunnen blijven toepassen, of dat zij liever een andere interventie inzetten. Als er na deze drie of vier dagen nog geen verandering in het slaap- en huilgedrag is, wordt met ouders besproken of een andere interventie wordt ingezet, of worden ouders verwezen.
In Nederland wordt deze methode uitgelegd in een boekje voor ouders (de “Schregardus”-methode).[157] Hierin krijgen ouders ook advies voor de omgang met het kind overdag. Ook wordt de methode kort uitgelegd in de Triple P folder voor ouders van peuters met slaapproblemen als de “Directe aanpak”.
De werkgroep beveelt aan dat wanneer op voorhand ingeschat wordt dat ouders deze methode niet gaan volhouden doordat er te weinig draagkracht of sociaal netwerk is, niet voor deze methode gekozen dient te worden. Deze methode wordt ook afgeraden indien sprake is van psychiatrische problematiek bij ouders, adoptiekinderen en veel scheidingsangst bij het kind.
Hoewel sommige ouders, vaak na veel andere interventies te hebben uitgeprobeerd, voor deze techniek kiezen, zien andere ouders deze interventie niet zitten. Zij willen hun kind niet alleen laten huilen. Voor deze ouders zijn er alternatieve vormen van uitdoving (zie hieronder).
Uitdoving met aanwezigheid van de ouders
Een variant op ongemodificeerde uitdoving is uitdoving met aanwezigheid van de ouders. Hierbij blijven de ouders in de kamer van het kind tijdens bedtijd, maar reageren niet op het kind en zijn/haar gedrag. Deze interventie wordt vaak gekozen als scheidingsangst verantwoordelijk is voor de slaapproblemen. Deze methode wordt kort uitgelegd in de Triple P folder voor ouders van peuters met slaapproblemen als de “zachte aanpak”. Een variant op deze vorm van uitdoving is dat ouders elke nacht verder van het bed van het kind gaan zitten. Sommige ouders vinden deze werkwijze meer acceptabel en zijn hierdoor meer in staat om consequent te zijn. In het boekje voor ouders “slaapproblemen de baas” van José Sagasser wordt een variant van deze aanpak beschreven als het “Stappenplan”.
Ook bij deze interventie is het belangrijk dat professionals met ouders afspreken op korte termijn (bijv. de volgende dag) contact op te nemen om te bespreken hoe de nacht is verlopen. De interventie is meestal binnen een week effectief. Daarna kan de ouder de aanwezigheid gaan afbouwen, bijvoorbeeld door alleen in de kamer aanwezig te zijn bij het inslapen, en daarna volledig afwezig te zijn zodat het kind leert alleen in de kamer te slapen. Als er na een week geen verbetering is, wordt met ouders besproken of een andere interventie wordt ingezet, of worden ouders verwezen.[20][130]
Graduele uitdoving
De term graduele uitdoving wordt gebruikt voor verschillende technieken.[20][130] Meestal worden ouders geïnstrueerd om huilen en drammen (tantrums) rond bedtijd te negeren voor een bepaalde tijd. De tijd tussen de aanwezigheid van de ouders wordt meestal bepaald op basis van de leeftijd en temperament van het kind, maar ook op basis van de inschatting van de ouders over hoe lang zij het huilen kunnen verdragen. Ouders kunnen hierin een vast schema hanteren, zoals elke 5 minuten naar het kind gaan (“minimaal checken”). Een variant van deze methode wordt in het boekje voor ouders “Slaapproblemen de baas” van José Sagasser beschreven als de “Kiekeboe-methode”. Bij “incrementele” graduele uitdoving neemt de tijd tussen de intervallen toe gedurende dezelfde nacht, of gedurende de opeenvolgende nachten (zie Tabel 1). De tijd dat ouders bij hun kind zijn duurt meestal 15 seconden tot een minuut. Aan ouders wordt uitgelegd hun aandacht te minimaliseren wanneer zij bij hun kind zijn, zodat ze aandacht vragend gedrag niet in de hand werken en het probleemgedrag niet wordt versterkt.[20][130] Deze methode wordt ook kort uitgelegd in de Triple P folder voor ouders van peuters met slaapproblemen als de “geleidelijke aanpak” en in het boekje “Slaap kindje, slaap” van dr. Eduard Estivill.
Het doel van graduele uitdoving is dat kinderen langzaamaan “zelf-troostend” gedrag ontwikkelen, zodat ze leren zelf in slaap te vallen zonder ongewenste gewoontes rond het slapen gaan (zoals in slaap wiegen door de ouder). Zodra dit zelfregulerende gedrag ontwikkeld is, is het kind in staat om zelfstandig in slaap te vallen en ook ’s nachts als hij wakker wordt weer zelf in slaap te vallen. Graduele uitdoving reduceert significant bedtijd problematiek en nachtelijk wakker worden.[20][130] In een Australische RCT naar een gedragsmatige slaapinterventie, bleek dat er na vijf jaar na de interventie geen significant verschil was tussen de controlegroep en de interventiegroep op alle uitkomstmaten, waaronder cortisolwaarden en slaapproblemen.[162]
Vergelijkbaar met de hierboven beschreven technieken adviseren we professionals met ouders af te spreken dat zij op korte termijn (bijv. de volgende dag) contact opnemen om te bespreken hoe de nacht is verlopen. De interventie is meestal binnen een week effectief. Daarna kan de ouder de aanwezigheid gaan afbouwen, bijvoorbeeld door alleen in de kamer aanwezig te zijn bij het inslapen, en daarna volledig afwezig te zijn zodat het kind leert alleen in de kamer te slapen. Als er na een week geen verbetering is, wordt met ouders besproken of een andere interventie wordt ingezet, of dat ouders worden verwezen.
Tabel 1. Schema voor het aantal minuten van wachten voordat ouders reageren op het huilen van hun baby bij het graduele uitdoving protocol.
|
Nacht |
duur 1e keer wachten |
duur 2e keer wachten |
duur 3e keer wachten |
duur van de daaropvolgende keren wachten |
|
1e nacht |
2 | 4 | 6 | 6 |
|
2e nacht |
3 | 5 | 7 | 7 |
|
3e nacht |
5 | 10 | 15 | 15 |
|
4e nacht |
10 | 15 | 20 | 20 |
|
5e nacht |
15 | 20 | 25 | 25 |
|
6e nacht |
20 | 25 | 30 | 30 |
|
7e nacht |
25 | 30 | 35 | 35 |
Positieve routines en het geleidelijk veranderen van de bedtijd.
Positieve bedtijd routines zijn gewoonten die ouders hanteren bij het naar bed gaan en die gekenmerkt worden door rustige activiteiten die het kind leuk vindt.[20][130] Met ‘geleidelijk veranderen van de bedtijd wordt de bedtijd tijdelijk verschoven naar het moment waarop het kind normaal gesproken in slaap valt, om ervoor te zorgen dat het kind snel in slaap valt als het naar bed wordt gebracht. Hierdoor wordt snel het in slaap vallen gekoppeld aan positieve ouder-kind interacties rond bedtijd. Ook wordt het kind voor afgesproken periodes uit bed gehaald als het kind na 15 minuten niet in slaap valt (bijvoorbeeld voor 30 minuten). Zodra de juiste gedragsketen bereikt is en het kind gemakkelijk in slaap valt (binnen 15-20 minuten), wordt de bedtijd weer naar voren geschoven met 15 tot 30 minuten per dag totdat de gewenste bedtijd bereikt is. Er wordt een vaste tijd van opstaan afgesproken en slapen overdag is niet toegestaan, met uitzondering van bij de leeftijd passende slaapjes.
Deze methode kan het beste worden toegepast bij kinderen vanaf ongeveer 1,5 jaar. Deze strategie laat de bedtijd van het kind aansluiten bij zijn/haar natuurlijke inslaaptijd. Er wordt gebruik gemaakt van stimulus controle technieken, wat een werkzaam element is van gedragsverandering. Deze interventie richt zich meer op het vergroten van wenselijk gedrag en controle van affectief gedrag, dan te focussen op verminderen van ongewenst gedrag, zoals gedaan wordt bij de uitdoving strategie.
Onderzoek laat zien dat positieve routines snel en effectief zijn om opstandig gedrag rond bedtijd (‘tantrums’) te verminderen.[20][130]
Vergelijkbaar met de hierboven beschreven technieken adviseren we professionals met ouders af te spreken dat zij op korte termijn (bijv. de volgende dag) na de start van de interventie contact opnemen om te bespreken hoe de nacht is verlopen. Als er na een week geen verbetering is, wordt met ouders besproken of een andere interventie wordt ingezet, of dat ouders worden verwezen.
Massagetherapie
Er zijn enkele aanwijzingen dat massagetherapie een positief effect heeft op de slaap van baby’s en jonge kinderen met autisme. [131][132][133]
6.1.3 Basisschoolleeftijd (vanaf 6 jaar)
Bedtijd pas
Bij kinderen van schoolgaande leeftijd spelen er vaak problemen rond het naar bed gaan. Zo weigeren sommige kinderen naar bed te gaan, of willen zij steeds uit bed komen. De gedragsmatige aanpak die hierbij wordt ingezet is o.a. het ongewenste gedrag van het weigeren om naar bed te gaan negeren en het gewenste gedrag belonen.[135][136] Een van de onderzochte methodes maakt gebruik van een “bedtijd pas”. Kinderen krijgen van de ouders een pas die ze kunnen inruilen tegen bijv. de ouder komt één keer naar de slaapkamer, of het is één keer toegestaan om uit bed te komen. Daarna levert het kind de pas in en wordt het roepen om de ouder genegeerd. Het gewenste gedrag wordt beloond met bijvoorbeeld een sticker systeem.[137]
Vergelijkbaar met de hierboven beschreven technieken adviseren we professionals met ouders af te spreken dat zij de volgende dag na de start van de interventie contact opnemen om te bespreken hoe de nacht is verlopen. Als er na een week geen verbetering is, wordt met ouders besproken of een andere interventie wordt ingezet, of dat ouders worden verwezen.
6.1.4 Adolescenten
Lichttherapie
In een studie kregen adolescenten met een slaapstoornis Cognitieve gedragstherapie (CGT) met lichttherapie.[138] Adolescenten werd geadviseerd de lichttherapie in de ochtend toe te passen door zich bloot te stellen aan natuurlijk zonlicht of een felle lamp (>10000 lux) voor minimaal een half uur. De lichttherapie wordt gestart bij het huidige tijdstip waarop de adolescent natuurlijk ontwaakt. Vervolgens wordt dit tijdstip elke 3 dagen met 1 uur vervroegd tot het gewenste tijdstip van opstaan is bereikt. In de zomer kan de lamp van >10.000 lux vervangen worden door natuurlijk daglicht. In vergelijking met de wachtlijstgroep waren er middelmatige tot grote effecten op de nameting voor de CGT met lichttherapie groep, waaronder positieve effecten op de duur van het in slaap vallen, eerder in slaap vallen, tijd van ontwaken, totale slaapduur (op schooldagen), wakker worden na het in slaap vallen en vermoeidheid. Ook na 6 maanden bleven er kleine tot grote verbeteringen zichtbaar voor de interventiegroep. Het effect van lichttherapie werd ook aangetoond bij kinderen met een verstandelijke handicap en adolescenten met een achtergrond van alcoholmisbruik.
Lichttherapie kan worden toegepast binnen de JGZ door een getrainde professional bij adolescenten met een verstoord biologisch klokritme. De JGZ professional kan ook verwijzen naar een Slaapcentrum waar lichttherapie wordt toegepast.
Cognitieve gedragstherapie bij Insomnia (CGT-i)
CGT–i bestaat uit een combinatie van stimuluscontrole, beperking van de tijd in bed, slaaphygiëne, relaxatie en cognitieve herstructureren. CGT-i wordt toegepast als effectieve therapie bij volwassenen. De techniek wordt ook toegepast bij adolescenten met een insomnie. In een studie in Nederland werd bij adolescenten CGT-i aangeboden via internet of in een groepssessie via het programma “Slim slapen”.[139] Beide vormen lieten significante verbeteringen zien, met een middelmatig tot groot effect, op de duur van het inslapen, wakker worden, slaapduur en de slaapefficiëntie. Een uitgebreide omschrijving van CGT-i bij adolescenten is te vinden in het boek Protocollaire behandelingen voor kinderen en adolescenten met psychische klachten, deel 2, van Braet en Bögels. Een getrainde JGZ professional kan de CGT-i, al dan niet in groepsverband uitvoeren. De JGZ professional kan ook verwijzen naar een slaapcentrum of een cognitief gedragstherapeut en/of een GZ psycholoog K&J/orthopedagoog-generalist die CGT-i toepast.
Mindfulness
Er werden twee studies gevonden naar het effect van op mindfulness gebaseerde stressreductie, in combinatie met cognitieve therapie, slaap hygiëne voorlichting, lichttherapie en stimulus controle instructies, op slaapproblemen bij adolescenten.[154][155]
In een studie kregen 55 adolescenten die behandeld werden voor alcoholmisbruik en die slaapproblemen rapporteerde de therapie. Op zelf-gerapporteerde uitkomsten was er een significante vermindering van slaperigheid, zorgen maken, mentale gezondheidsstress na afloop van de behandeling en was er een significante verbeteringen in aspecten van slaapkwaliteit bij personen die de behandeling helemaal doorliepen.
In een andere studie waarbij hetzelfde protocol werd toegepast als in de studie van Britton et al.[155], met daaraan toegevoegd het omgaan met piekeren tijdens bedtijd, werden bij tien meisjes positieve effecten gevonden van de behandeling op slaap.[156] Bij beide studies was er geen controlegroep.
Mindfulness kan worden toegepast binnen de JGZ door een getrainde professional. De JGZ professional kan ook verwijzen naar een eerstelijns kind- en jeugdpsycholoog en/of orthopedagoog-generalist die een contract hebben via de gemeente en die Mindfulness toepassen.
Valeriaan
Er werd slechts één kleine RCT studie gevonden naar valeriaan bij vijf kinderen van 7-14 jaar met een intellectuele achterstand. Er werd een significant verschil gevonden op de ervaren slaapkwaliteit, in het voordeel van de valeriaan.
6.2 Slaaptips voor kinderen
De volgende aanbevelingen helpen u en uw kind om zo goed mogelijk te slapen en
maken het gemakkelijker in slaap te vallen en door te slapen.
- Probeer regelmatige bedtijden aan te houden voor zowel doordeweeks als ook in het weekend. Spreek aan het begin van het schooljaar een passende bedtijd af en laat uw kind ieder jaar 15 minuten later naar bed gaan. In het weekend mag uw kind uiteraard iets later naar bed en in de ochtend wat langer slapen, maar probeer hier maximaal 1,5 uur verschil in te laten zitten tussen schooldagen en weekenddagen/vakanties.
- Biedt een positief en rustig bedtijdritueel. Maak het na het avondeten alvast donker in huis en doe alle digitale apparaten uit 1,5 uur voor bedtijd. Deze geven namelijk te veel (blauw) licht, waardoor kinderen later in slaap vallen en onrustiger slapen. Ook liever geen t.v. aan. Muziek luisteren, knutselen, kleuren, lezen, praten en/of een bord-/kaartspelletje met een klein lampje aan is prima. Zorg er ook voor dat uw kind niet tot te laat doorgaat met huiswerk, dit houdt de hersenen te actief waardoor uw kind mogelijk moeilijk in slaap valt. Probeer zelf ook te stoppen met werken,leg digitale apparaten weg en geniet even van dit rustmoment met uw kind.
- Slaapkamer: Zorg ervoor dat de slaapkamer niet te warm is (tussen 16-18 graden) en goed geventileerd is. De kamer moet voldoende donker zijn, vooral in de zomer is dit handig, anders valt uw kind pas laat in slaap en is het bij zonsopkomst alweer wakker! Is uw kind bang in het donker, dan mag er best een nachtlampje aan of een lampje op de gang bijvoorbeeld. Zet geen t.v. in de kamer en zorg ervoor dat tijdens het slapen alle digitale apparatuur in een andere kamer ligt. Deze verstoren namelijk de nachtrust, ook al staan ze op ‘stil’.
- Drinken/eten: Het is beter dat uw kind geen cafeïnehoudende dranken meer neemt in de laatste 4 uur voor het naar bed gaan. Cafeïne zit onder andere in cola, ice-tea, (zwarte) thee, chocolade (dus ook chocolademelk), energydrinks en koffie. Zorg ervoor dat uw kind gezond eet en op regelmatige tijden. Leg een kind niet vlak na de avondmaaltijd op bed, dit kan de slaap verstoren.
- Dutjes: De meeste kinderen van 4 jaar en ouder hebben geen middagdutje meer nodig. Is uw kind toch erg moe na school, mag het gerust maximaal 30 minuten slapen, tenzij hij/zij dan ‘s avonds niet meer op tijd in slaap komt, dan worden dutjes afgeraden.
- Lichamelijke activiteiten: laat uw kind iedere dag buiten spelen, zodat hij/zij voldoende beweegt en daglicht ziet. Hierdoor vallen ze ‘s avonds sneller in slaap en slapen ze dieper. Laat oudere kinderen echter niet te laat op de avond sporten/trainen, omdat ze hierna niet direct in slaap kunnen vallen.
Tijdens het ontwikkeltraject van de richtlijn werd geen voorlichtingsmateriaal voor ouders en jongeren gevonden wat zowel inhoudelijk klopt, als ook voor alle ouders en jongeren geschikt is, inclusief ouders en jongeren met lage gezondheidsvaardigheden. Deze bijlage betreft een inhoudelijk basisoverzicht met slaaptips voor ouders van jongere kinderen. Deze tips zijn ontwikkeld door het MCH. Pharos benadrukt dat het voorlichtingsmateriaal niet geschikt is voor alle ouders en jongeren en dat aanpassingen wat betreft vormgeving en taalgebruik gewenst zijn.
6.3 Slaaptips voor pubers en adolescenten
De volgende tips maken de kwaliteit van je slaap beter en zorgen ervoor dat je makkelijk in slaap valt: Regelmatig slaap-/waakschema: Ga naar bed en sta op omstreeks dezelfde tijd elke dag, zowel
op doordeweekse dagen als in het weekend. Pubers hebben nog wel een slaapbehoefte van gemiddeld 8,5 a 9 uur, dus in het weekend mogen zij zeker uitslapen, maar probeer maximaal 2 uur later dan doordeweeks op te staan. Dus liever niet tot in de middag uitslapen, want dan kom je zondagavond niet op tijd in slaap!
- Doe 1,5 uur voor bedtijd alle digitale apparaten uit en laat niet je telefoon/tablet in de slaapkamer liggen.
- Doe ook geen t.v. aan in de kamer. Het (blauwe) licht dat het scherm geeft zorgt ervoor dat je pas later dan normaal slaperig wordt en zorgt ervoor dat je onrustiger slaapt en vaker wakker wordt tussendoor.
- Dutjes: Als je moeite hebt met in slaap vallen ’s avonds, kun je beter overdag
niet slapen. Alles wat je overdag slaapt, lig je ’s nachts wakker! - Zonlicht: Ga elke dag naar buiten, vooral in de ochtenden, omdat blootstelling aan zonlicht of helder licht helpt om de biologische interne klok in de pas te houden en je een wakker gevoel geeft.
- Beweging: beweeg regelmatig, liefst buiten in voldoende daglicht. Beweging maakt je lichaam moe, waardoor je sneller in slaap valt en dieper slaapt. Ga echter niet te laat in de avond sporten, het duurt namelijk altijd even voordat je dan in slaap kunt vallen en dan wordt het al snel te laat.
- Slaapkamer: Zorg voor een comfortabele slaapkamer die donker en stil is. Zorg er ook voor dat het niet te warm is (tussen 16-18 graden) en goed geventileerd wordt.
- Bed: gebruik je bed alleen om in te slapen en niet om in te studeren, lezen of muziek in te luisteren.
- Voeding: eet gezond en op regelmatige tijden (ontbijt, lunch en avondeten). Ga niet direct na een warme maaltijd in bed liggen, hierdoor slaap je onrustiger of krijg je buikpijn. Probeer minimaal 1 uur er tussen te laten zitten. Ga echter ook niet met honger slapen, eet bijv. nog wat fruit in de avond of yoghurt. • Cafeïne: vermijd het eten of drinken van producten die cafeïne bevatten in de late middag en avond. Hieronder vallen bijvoorbeeld: cola, ice-tea, koffie, thee en chocolade (-melk), maar ook energiedrankjes zoals Red Bull.
- Alcohol/drugs: het gebruik van alcohol/drugs verstoort de slaap en veroorzaakt waakperiodes tijdens de nacht.
- Roken: roken verstoort de slaap. Stop met roken in het laatste uur voor het naar bed gaan.
- Slaapmiddelen: gebruik geen slaappillen, melatonine of andere vrij verkrijgbare slaaphulpmiddelen. Deze middelen verstoren de slaap op verschillende manieren en zorgen voor het terugkomen van het slaapprobleem als je er mee stopt.
- Ga niet slaperig achter het stuur zitten: Tieners lopen het grootste risico om achter het stuur in slaap te vallen. Als je niet genoeg geslapen hebt, ga dan niet auto rijden of op de fiets/scooter. Ongelukken gebeuren vooral midden op de dag en ’s nachts.
- Merk je dat je iedere avond veel ligt te denken of je zorgen maakt over dingen? Blijf er niet mee zitten, bespreek het met je ouders of een mentor.
Tijdens het ontwikkeltraject van de richtlijn werd geen voorlichtingsmateriaal voor ouders en jongeren gevonden wat zowel inhoudelijk klopt, als ook voor alle ouders en jongeren geschikt is, inclusief ouders en jongeren met lage gezondheidsvaardigheden. Deze bijlage betreft een inhoudelijk basisoverzicht met slaaptips voor jongeren. Deze tips zijn ontwikkeld door het MCH. Pharos benadrukt dat het voorlichtingsmateriaal niet geschikt is voor alle ouders en jongeren en dat aanpassingen wat betreft vormgeving en taalgebruik gewenst zijn.
6.4 Sensitief opvoeden en een kind dat niet slaapt (uitdoving)
Slaapproblemen bij kinderen komen relatief vaak voor en kunnen zowel voor het kind zelf als voor hun ouders nadelige gevolgen hebben (zie Subsubsectie Slaapproblemen).
Eén van de technieken die ingezet kan worden als interventie bij slaapproblemen bij kinderen is extinctie; het laten uitdoven van ongewenst gedrag en het belonen van gewenst gedrag (zie sectie Begeleiden en behandelen voor een uitgebreide beschrijving van uitdovingstechnieken). Uit onderzoek naar de verschillende uitdovingstechnieken bij (jonge) kinderen blijkt dat zij effectief zijn voor het verminderen van slaapproblemen.[20][116][130][187]
In de (internationale) media, maar ook in de wetenschappelijke literatuur wordt al jaren discussie gevoerd over de vraag of het “laten huilen”, wat onderdeel is van de uitdovingstechnieken, van een jong kind schadelijk is.[112][116][158][160][187][188][189][190][191][192][193][194] Tegenstanders van deze techniek stellen dat het alleen laten huilen van een baby op twee manieren schadelijk zou kunnen zijn. Ten eerste stellen zij dat het laten huilen nadelige gevolgen heeft voor het stressniveau van de baby en dat het daarmee langdurige schadelijke gevolgen kan hebben. Ten tweede stellen tegenstanders dat ouders die niet reageren op het huilen van hun baby niet sensitief en responsief reageren, wat volgens hen schadelijk zou zijn voor de ontwikkeling van een goede gehechtheidsrelatie tussen ouder en baby. In deze bijlage wordt de wetenschappelijke literatuur rond beide standpunten samengevat, evenals de wetenschappelijke evidentie voor alternatieven. Op basis van deze literatuur heeft de werkgroep geconcludeerd dat uitdovingstechnieken in principe niet schadelijk zijn, mits correct toegepast en adequate ondersteuning aan ouders wordt geboden.
6.4.1 Randvoorwaarden voor het toepassen van uitdoving
We adviseren JGZ professionals om uitdovingstechnieken in te zetten als ouders een slaapprobleem ervaren met hun baby vanaf ongeveer 6 maanden (en naar inschatting van de professional), nadat zij a) samen met ouders een uitgebreide anamnese af hebben genomen van de oorzaak van het slaapprobleem en nagegaan zijn of er geen fysieke problemen ten grondslag liggen aan het slaapprobleem, b) ouders hebben geadviseerd over een gezonde slaaphygiëne, en c) nadat zij met ouders overlegd hebben of ouders het toepassen van het “laten huilen” van hun baby wenselijk vinden of niet. We adviseren professionals daarnaast om ook naar het gedrag en de relatie tussen ouder en kind overdag te kijken. Indien de interventies correct worden toegepast, blijken zij vaak op zeer korte termijn te werken. We adviseren professionals om met ouders af te spreken om meteen na de eerste nacht contact op te nemen om te vragen hoe de nacht is verlopen. Uit ervaring van werkgroepleden blijkt dat het slaapprobleem in de meeste gevallen na maximaal drie dagen is verholpen. Als er in de loop van deze drie dagen geen verandering is, is het belangrijk om samen met ouders te bespreken hoe zij het toepassen van de interventie hebben ervaren en om te kijken of zij de interventie zoals bedoeld willen blijven toepassen, of dat zij liever een andere interventie inzetten. Als er na deze drie of vier dagen nog geen verandering in het slaap- en huilgedrag is, worden ouders doorverwezen.
Daarnaast zijn er verschillen tussen wat ouders als slaapprobleem ervaren. Voor de ene ouder is het geen probleem dat een baby vaak ’s nachts wakker wordt, terwijl het voor de andere ouder wel als een slaapprobleem wordt ervaren. Rekening houden met de cultuur van ouders en individuele verschillen is cruciaal bij het ondersteunen van ouders zodat zij hun eigen keuzes en gedrag kunnen accepteren en er een gevoel van competentie over kunnen ontwikkelen.[192]
6.4.2 Stress
Zoals eerder genoemd zijn tegenstanders van mening dat het laten huilen van baby’s, wat onderdeel is van de uitdovingstechnieken, veel stress geeft, en dat deze stress schadelijk is voor de gezondheid.
Ten eerste is het belangrijk om te benoemen dat stress niet altijd slecht is. Ook leuke gebeurtenissen kunnen een lichamelijke stressreactie geven, zoals het winnen van de loterij. In reactie op stress maakt het lichaam het hormoon cortisol aan. Het aanmaken van cortisol is een normale reactie van het lichaam en helpt het brein en het lichaam om effectief om te gaan met nadelige situaties. Als het het lichaam niet lukt om de cortisolafgifte te stoppen of als de stress chronisch is, kunnen er lange termijn effecten optreden zoals een onderdrukt immuunsysteem, en draagt het bij aan o.a. het metabool syndroom, verlies van botmineraal, en spieratrofie.[196] Er is echter nog niet duidelijk bij welke hoogte en voor welke duur van een verhoogd cortisolniveau de voorgenoemde schadelijke effecten kunnen optreden.
Cortisolniveaus bij baby’s
In de afgelopen jaren is steeds meer onderzoek gedaan naar stressniveaus bij baby’s. Cortisolniveaus bij baby’s zijn relatief gemakkelijk vast te stellen in speeksel. Bij baby’s worden twee typen onderzoek gedaan naar cortisol, namelijk naar de cortisolniveaus gedurende de dag (of meerdere dagen), om te vergelijken of de cortisolniveaus langdurig hoog zijn, of naar de cortisolniveaus in reactie op een stressvolle gebeurtenis.
Het meeste onderzoek is gericht op chronische stress gedurende de jeugd. Meerdere onderzoeken tonen aan dat chronische stress schadelijk is voor de gezondheid op latere leeftijd.[197] Bijvoorbeeld chronische stress door misbruik, verwaarlozing, dood van de ouder, depressie bij de ouder, conflict in families of meerdere transities van verzorgers en armoede, beïnvloeden allen het biologische systeem.
Daarnaast zijn er enkele onderzoeken gedaan naar de cortisolniveau-reactie na een stressvolle gebeurtenis.[198] Bijvoorbeeld het verschonen van de luier, een lichamelijk onderzoek, in bad gaan, een hielprik, een vaccinatie, een half uur durende scheiding van de moeder, etc. De meeste fysieke stressoren geven een verhoogde cortisolreactie, terwijl de meeste psychische stressoren geen verhoogde cortisolreactie geven. Wat de gevolgen op de gezondheid zijn van deze kortdurende verhoogde stressreacties is niet bekend. Ook is niet direct onderzocht wat de gevolgen zijn van het huilen van baby’s op de gezondheid en cortisolniveaus.
Cortisolniveaus na het laten huilen
Er werden tot op heden drie onderzoeken gedaan naar cortisolniveaus na het laten huilen van baby’s in het kader van uitdoving bij slaapproblemen. In één onderzoek werd bij 25 baby’s van 4-6 maanden, waarvan de ouders aangaven dat er slaapproblemen waren, ongemodificeerde uitdoving toegepast door verpleegkundigen tijdens een ziekenhuisopname.[161] Cortisolniveaus werden afgenomen bij moeder en baby op dag één en dag drie van de slaapinterventie, zowel voorafgaand aan de slaaproutine, als 20 minuten na het in slaap vallen.
De cortisolniveaus van de baby’s waren niet significant hoger voor het begin van de slaaproutine, tot na de slaaproutine, zowel op dag één, als na dag drie. Tijdens de eerste dag van het uitdovingsprogramma waren cortisolniveaus van de moeder en baby nog positief geassocieerd, op dag drie van het programma waren de cortisolniveaus van de moeder en baby niet meer met elkaar geassocieerd. De baby’s reageerden na drie dagen zichtbaar minder verontrust bij het in slaap vallen (o.a. minder huilen), maar de cortisolniveaus bleven even hoog als op dag één. Zonder de zichtbare verontrustte reactie van de baby, ging het cortisolniveau van de moeder naar beneden op dag drie. Met andere woorden, de cortisolniveaus van moeder en baby waren niet meer op elkaar afgesteld.
Bij deze studie zijn een aantal kanttekeningen te maken voordat de conclusie kan worden getrokken dat uitdoving een schadelijk effect heeft. Eén van de kanttekeningen is dat de baby’s in deze studie erg jong waren, vanaf 4 maanden oud. In een reactie op dit artikel adviseren Price, Hiscock en Gradisar6 om gedragsinterventies pas toe te passen als kinderen in staat zijn tot het begrijpen van “objectpermanentie”, vanaf ongeveer 6 maanden. Zoals eerder benoemd, treden er bij langdurig verhoogde cortisolniveaus schadelijke effecten op, maar het is nog onduidelijk bij welke hoeveelheid en duur van verhoogde cortisolniveaus deze schadelijke effecten optreden. Dit onderzoek geeft geen conclusie of de cortisolniveaus na de interventie langdurig verhoogd waren en of er bij de gemeten cortisolniveaus schadelijke effecten optreden.
Het enige onderzoek wat gedaan is naar de lange termijn effecten van uitdoving geeft een aanwijzing dat het niet schadelijk is. In een RCT werden de lange termijn effecten van uitdoving bij slaapproblemen onderzocht in Australië.[162] In deze studie participeerden ouders van 326 baby’s van 7 maanden met door ouders gerapporteerde slaapproblemen. De interventiegroep ontving van een verpleegkundige het advies om uitdoving (gradueel of de stap-voor-stap methode) toe te passen. In de controlegroep ontvingen zij zorg zoals die normaal geboden werd bij slaapproblemen door verpleegkundigen. Een jaar na afloop van de interventie bleek uitdoving effectief voor het verminderen van slaapproblemen. Echter, op de leeftijd van 6 jaar was er geen verschil meer tussen de interventie en controlegroep, waaronder geen verschil in slaapproblemen, cortisolniveaus, emotionele en gedragsproblemen, gezondheid-gerelateerde kwaliteit van leven, de ouder-kind relatie, gehechtheid, depressiescores van de moeder en opvoedingsstijl. Ook dit onderzoek heeft methodologische tekortkomingen: zo is onduidelijk of ouders in de interventiegroep de uitdoving daadwerkelijk hebben toegepast, en is de groep waar cortisol bij werd gemeten na 6 jaar mogelijk te klein om een effect te detecteren.
In een zeer recente studie werden 43 baby’s van 6-16 maanden met door ouders gerapporteerde slaapproblemen verdeeld over drie groepen; een controlegroep en twee interventiegroepen.9 In de ene interventiegroep kregen ouders de instructie graduele uitdoving toe te passen, en in de andere interventiegroep werd het opschuiven van de bedtijd toegepast. Er werden bij beide interventies significante effecten gevonden voor de duur van het in slaap vallen, het aantal keren ’s nachts wakker worden, en wakker worden na het in slaap vallen, waarbij er grote afnames werden waargenomen wat betreft de duur van het in slaap vallen in de graduele uitdoving groep en ook in de verschoven bedtijd groep. Ook was er een grote afname van het aantal keren ’s nachts wakker worden en wakker worden na de start van de slaap bij graduele uitdoving.
In deze studie werd ook cortisol gemeten, zowel voor de interventie, een week na de interventie, na drie en na twaalf maanden. Er was een kleine tot middelgrote afname van cortisol bij graduele uitdoving en het opschuiven van de bedtijd, in vergelijking met de controlegroep.
Het stressniveau van de moeder ging in beide interventiegroepen naar beneden, maar er werden geen verschillen in gemoedstoestand gevonden. Na 12 maanden waren er geen significante verschillen in emotionele en gedragsproblemen en ook geen verschillen tussen een veilige en onveilige gehechtheidsstijl tussen de groepen.
Conclusie
De onderzoeken die gedaan zijn naar de gevolgen van uitdoving hebben allen methodologische tekortkomingen. Meer robuust onderzoek zal moeten aantonen wat de gevolgen zijn van het toepassen van uitdoving. Ook moet worden nagegaan wat de gevolgen zijn van alternatieve interventies bij slaapproblemen. Niet effectieve methoden die het slaapprobleem niet verminderen kunnen ook schadelijke gevolgen hebben. Hoewel sommige slaapproblemen vanzelf overgaan, kunnen niet opgeloste slaapproblemen ernstige gevolgen hebben voor zowel ouder (bijv. depressie en relatieproblemen) als het kind (bijv. emotionele- en gedragsproblemen). Bovendien blijken slaapproblemen zelf bij kinderen ook gerelateerd te zijn aan verhoogde cortisolniveaus.[132]
6.4.3 Hechtingsrelatie
Onderzoek naar de gehechtheidsrelatie tussen ouder en kind toont aan dat het belangrijk is dat ouders sensitief en responsief reageren op hun baby. Kinderen met een problematische gehechtheidsrelatie hebben een hoger risico op internaliserende en externaliserende gedragsproblemen. In de Richtlijn Problematische gehechtheid, geschreven voor professionals in de jeugdzorg, staat beschreven hoe ouders gestimuleerd kunnen worden sensitief en responsief om te gaan met hun kind.
Er is weinig onderzoek gedaan naar het directe effect van uitdoving in het kader van slaapproblemen op de hechtingsrelatie. Twee van de hierboven beschreven onderzoeken namen ook de gehechtheidsrelatie als uitkomstmaat en vonden hierop geen effect van uitdoving.[162][190]
Wel zijn er een behoorlijk aantal onderzoeken gedaan waarin wordt aangetoond dat een verstoorde hechtingsrelatie vaker voorkomt bij kinderen met slaapproblemen,[199][200][201][202][203][204][205] hoewel andere onderzoeken geen relatie vonden tussen de hechtingsrelatie en slaapproblemen bij kinderen.[206][207] Geen van deze onderzoeken levert bewijs voor een causaal verband, het is dus onbekend of de slaapproblemen een verstoorde hechtingsrelatie veroorzaken, of dat een verstoorde hechtingsrelatie resulteert in slaapproblemen.
Conclusie
Er is enig bewijs dat slaapproblemen vaker voorkomen bij een verstoorde gehechtheidsrelatie. Echter, er is geen causaal bewijs, het is dus niet mogelijk om te spreken van een oorzakelijke relatie. Er is ook geen bewijs dat interventies die ingezet worden bij slaapproblemen de hechtingsrelatie beïnvloeden.
Naast onderzoek naar de hechtingsrelatie is er onderzoek gedaan naar andere aspecten van sensitief en responsief opvoeden en hoe ouders omgaan met hun kind rond het naar bed gaan. Bijvoorbeeld naar zelfregulatie bij het inslapen, betrokkenheid van de ouder ’s nachts en de emotionele beschikbaarheid van de ouder.
Zelfregulatie en interactie tijdens de nacht
Onderdeel van de discussie rond sensitief en responsief ouderschap richt zich op het aanleren van zelfregulatie bij het in slaap vallen vanaf een jonge leeftijd. Er wordt gesteld dat de capaciteit van zelfregulatie bij jonge kinderen zich ontwikkelt in de context van een veilige gehechtheidsrelatie. Door herhaalde succesvolle ervaringen van regulatie die door de ouder wordt ondersteund, wordt gedacht dat veilig gehechte kinderen deze vaardigheid in hun eigen repertoire opnemen, die vervolgens kan worden ingezet als de ouder afwezig is. Als deze theorie wordt toegepast in de context van slaap, kunnen verbeterde zelfregulatiecapaciteiten mogelijk vertaald worden in meer efficiënt zelftroostend gedrag bij het begin van het in slaap vallen en gedurende het ’s nachts wakker worden, en daarmee de capaciteit om sneller in slaap te vallen zonder tussenkomst van de ouder. Ouders die overbetrokken zijn bij het in slaap vallen van de baby zouden daarmee de zelfregulatie kunnen remmen.[41]
In een review van Sadeh3 1 en collega’s wordt een behoorlijke hoeveelheid literatuur samengevat rond het gedrag van ouders tijdens de nacht. Er wordt geconcludeerd dat minimale betrokkenheid van de ouder bij het in slaap vallen van het kind is gerelateerd aan betere slaap bij baby’s.
Uit twee longitudinale onderzoeken blijkt dat overbetrokkenheid van de moeder bij het in slaap vallen van het kind, op de leeftijd van 12 weken, minder optimale slaap voorspelde op de leeftijd van 18 maanden en 5 jaar.[208][209] Het aanmoedigen van autonomie (waaronder laten huilen) was geassocieerd met een langere slaapduur, maar niet met slaapproblemen op de leeftijd van 18 maanden.[208] Op de leeftijd van 5 jaar werd het aanmoedigen van autonomie niet apart geanalyseerd.[209]
Uit wat ouder onderzoek onder 288 moeders bleek dat excessief “actief fysiek troosten” (zoals in armen knuffelen) en verminderd “stimuleren van autonomie” (zoals laten huilen) waren geassocieerd met slaapproblemen bij baby’s van 13 maanden. Wat betreft de verandering in ontwikkeling in strategie tussen de leeftijd van 1 en 2 jaar bleek dat hoe later “stimuleren van autonomie” de meest gebruikte strategie werd, hoe groter de kans dat persistente slaapproblemen aanwezig waren. In het artikel wordt opgemerkt dat ouders in de “geen-slaapprobleem” groep ook veel gebruik maakten van actief fysiek troosten, maar dat dit werd uitgebalanceerd door een hoge mate van het stimuleren van autonomie. Moeders in de slaapprobleem-groep vertrouwden veel op actief fysiek troosten, wat ten koste ging van het stimuleren van autonomie. De balans tussen de twee strategieën bleek hierbij van belang.[210]
In een eveneens wat oudere studie onder 100 baby’s van 14-16 maanden bleek dat de relevante factoren voor samenhangende slaapproblemen waren (in volgorde van belangrijkheid): problematische cognities van de moeder wat betreft het stellen van grenzen, moeilijk temperament van het kind, angst-depressie van de moeder, ambivalente gehechtheidstijl, bepaald zorggedrag van de moeder waarbij zij met actief fysiek contact troost (in slaap knuffelen, op de bank of in het bed van de ouders troosten, een voeding geven).[203] Hoge initiële niveaus van slaapproblemen verklaarden voor een groot deel het voortbestaan van slaapproblemen. Echter, dit voortbestaan werd significant gemedieerd door de invloed van zowel problematische cognities van de moeder, temperament van het kind en actief fysiek troosten van het kind om het in slaap te laten vallen. Ambivalente gehechtheid had een kleine maar significante onafhankelijke bijdrage aan persistente problemen. Wat betreft discontinuïteit in slaapproblemen bij zuigelingen over de tijd, hadden zuigelingen die slaapproblemen ontwikkelden vaker ouders die hoge niveaus van actief fysiek troosten gebruikten, terwijl zuigelingen wiens slaapproblemen ophielden vaker moeders hadden met lage angst/depressie.
Uit recent onderzoek onder 84 kinderen bleek dat hogere niveaus van betrokkenheid van de ouders bij de slaap betere objectieve slaappatronen voorspelde voor kinderen met gegeneraliseerde angststoornis, maar juist slechtere slaap voor gezonde kinderen (zonder gegeneraliseerde angststoornis). Hoewel een oorzakelijke richting in de relatie vanuit deze data niet kan worden geconcludeerd, is het mogelijk dat overbetrokkenheid van ouders de zelfregulatie van baby’s alleen in sommige gevallen ondermijnt, zoals bij baby’s die zichzelf kunnen troosten.[211]
Niet uit alle onderzoeken blijkt een relatie tussen interactie tijdens de nacht en slaap; uit een onderzoek onder 45 moeders met een baby van 1 tot 24 maanden oud, bleek dat de tijd die moeders besteden aan de volgende gedragingen tijdens het ’s nachts wakker worden van de baby niet significant gerelateerd waren aan slaapproblemen: dicht-fysiek contact (dicht tegen het lichaam), los-fysiek contact (aanraken, maar niet tegen het lichaam houden), voeden, en stille activiteiten (in stilte spelen, interactie, lezen).[212]
Naast de mate van betrokkenheid tijdens de nacht werd ook gekeken naar het concept van emotionele beschikbaarheid van de moeder tijdens de nacht en de relatie met slaap. In een tweetal onderzoeken werd de emotionele beschikbaarheid gescoord in videobeelden, waarbij gebruik werd gemaakt van vier subschalen: sensitiviteit, structureren, niet-opdringerigheid en niet-vijandigheid. Wat betreft sensitiviteit kregen ouders geen lage (“slechtere”) score als zij niet reageerden op niet-verontrustende geluiden van het kind en als zij minder lang dan 1 minuut wegbleven als de baby huilde. Uit onderzoek onder 45 moeders met een baby bleek dat moeders die over het algemeen emotioneel beschikbaar waren tijdens de nacht was, minder vaak ’s nachts naar de baby gingen, de baby zelf ’s nachts minder vaak wakker werd en de ouders minder slaapproblemen bij hun kind ervaarden.[212] Op de leeftijd van 3 maanden hadden baby’s van emotioneel beschikbare moeders lagere cortisolniveaus tijdens de nacht. Uit nadere analyses bleek dat vooral moeders die hoog scoorden op de schaal “structureren” en “niet-opdringerigheid” baby’s hadden met lagere cortisolniveaus gedurende nacht.[213]
Naast onderzoek naar de relatie tussen interactie tijdens de nacht en slaap werd in twee andere onderzoeken gekeken naar de relatie tussen interactie tijdens de nacht en de gehechtheidsrelatie. Uit een kleinschalig onderzoek bleek dat onder 10 moeders die geen aandacht gaven bij het wakker worden van de baby (nadat de baby liet merken dat hij/zij wakker was), er geen significante verschillen waren tussen moeders met veilig en onveilig gehechte kinderen.[201] Moeders in de veilig gehechte groep hanteerden deze optie (geen aandacht) net iets vaker dan in de onveilige groep, maar dit verschil was niet significant. Onder 14 moeders die wel aandacht gaven aan het wakker worden van het kind en die een “oppakken en troosten” interactie hanteerden waren significant meer moeders met veilig gehechte kinderen dan moeders van onveilig gehechte kinderen. Tien andere baby’s werden ‘nachts niet wakker en bij tien andere baby’s hanteerden moeders verschillende technieken. Bij beide categorieën waren er geen significante verschillen tussen een veilige en onveilige gehechtheidsstijl van de moeders.
Ook uit ander onderzoek onder 550 moeders van baby’s bleek dat proximale (dicht bij het lichaam houden) en distale nachtelijke troosttechnieken (op afstand troosten) op de leeftijd van 2 maanden niet significant geassocieerd waren met gehechtheid op de leeftijd van 14 maanden.[204]
Conclusie
Er is enig onderzoek gedaan rond het stimuleren van zelfregulatie bij het in slaap vallen en het effect van overbetrokkenheid van ouders tijdens de nacht op slaapproblemen. De meeste onderzoeken wijzen in de richting dat het stimuleren van autonomie en minimale betrokkenheid van ouders bij het in slaap vallen beter is voor de slaap van het kind. Echter de resultaten zijn niet eenduidig en ook bij dit onderwerp blijkt het moeilijk te bepalen of er sprake is van een oorzakelijk verband. Daarnaast blijft het onduidelijk op welke leeftijd, met welke mate en met welke balans betrokkenheid en het stimuleren van autonomie precies een gunstig effect hebben op de slaap van het kind.
Minimale betrokkenheid tijdens de nacht en het stimuleren van autonomie, waaronder het laten huilen, lijken op het eerste gezicht misschien het tegenovergestelde van sensitiviteit en responsiviteit. Maar wat precies wel en niet onder een responsieve en sensitieve opvoeding moet worden verstaan (op welke leeftijd, met welke mate en welke balans) is evenmin wetenschappelijk onderbouwd. Een voorbeeld hiervan is dat in een onderzoek naar responsiviteit, tegen de verwachting in, bleek dat de frequentie van het niet reageren op huilen positief was geassocieerd met minder huilen in de maanden daarna.[214][215] Moeders van baby’s met een vermijdende gehechtheidsstijl reageerden bovendien sneller op het huilen dan moeders van baby’s met een veilige en ambivalente gehechtheidsstijl. De auteurs concluderen hierop dat reageren op alle signalen en huilen van baby’s a) praktisch niet haalbaar lijkt in het dagelijks leven en b) mogelijk niet altijd een adequate reactie is, omdat het ook overstimulatie kan zijn wat de ontwikkeling van veilige gehechtheid en autonomie kan beperken.
6.4.4 Alternatieven voor uitdoving
Er is weinig onderzoek gedaan naar andere interventies voor het verminderen van slaapproblemen bij jonge kinderen. Uit een review van 11 studies naar het verminderen van slaapproblemen bij baby’s van onder de 6 maanden, bleek er bij 8 studies een verbetering op slaapuitkomsten te zijn.2 De interventies die een focus hadden op het aanleren zelf in slaap te vallen bleken effectief. De interventies die een focus hadden op het gedrag van de moeder (zoals de slaaphygiëne van de moeder, relaxatie en het optimaliseren van opvoedondersteuning), hadden inconsistente effecten; uit één studie bleek dat de interventie effectief was, terwijl in een andere studie geen verschil werd gevonden. De enige onderzochte interventie waarbij de focus lag op consistent reageren en waarbij ouders werden gestimuleerd altijd te reageren op het huilen van het kind, bleek niet effectief voor het verminderen van slaapproblemen.[216] In deze studie waren de interventiegroep en de controlegroep echter niet goed te vergelijken. De controlegroep was een groep ouders die in de gemeenschap geworven werd en waarvan het onduidelijk is of deze ouders wel of geen ondersteuning kregen. De ouders in de interventiegroep hadden na de interventie significant hogere niveaus van competentie en zelfvertrouwen dan ouders in de controlegroep. Er waren geen significante verschillen tussen de groepen na vier weken wat betreft de duur van het troosten, het ’s nachts wakker worden van het kind en depressie en angst van de moeder.
Een andere interventie die geen gebruik maakt van uitdoving is “Positieve routines en het geleidelijk veranderen van de bedtijd”. Deze interventie blijkt vooral effectief voor problemen bij het in slaap vallen.[130][190] Bij deze interventie wordt de bedtijd tijdelijk verlaat, waardoor kinderen sneller inslapen en de juiste signalen van het in slaap vallen gekoppeld worden aan positieve ouder-kind interacties. Zodra de juiste gedragsketen is bereikt, kunnen ouders de bedtijd weer naar voren schuiven met 15 – 30 minuten per keer tot aan de gewenste bedtijd.
Op dit moment loopt er onderzoek naar andere interventies voor het verminderen van slaapproblemen waarbij geen gebruik wordt gemaakt van uitdoving. Zo beschrijven Whittingham en Douglas[217] dat zij een nieuwe interventie voor slaapproblemen ontwikkelden. Deze interventie ondersteunt volgens hen de flexibiliteit van ouders, zorg gebaseerd op de signalen van de baby en het vestigen van gezonde bio-psycho-sociale ritmes. Er zijn op dit moment nog geen onderzoeksresultaten bekend.
Samen in één bed slapen
Een andere alternatieve methode die op websites voor ouders die hun kind niet willen laten huilen wordt geadviseerd, is om het kind in het bed van de ouders te laten slapen. Uit onderzoek blijkt echter niet dat kinderen die bij de ouders in bed slapen minder slaapproblemen hebben. In een recente narratieve review van 659 artikelen onderzochten Mileva-Seitz en haar collega’s[218] de relatie tussen samen in één bed slapen en onder andere slaap(problemen). Bij alle studies is het de vraag of ouders die ervoor kiezen om samen in één bed te slapen met hun kind, daarmee slaapproblemen veroorzaken, of juist voor samen in één bed slapen kiezen omdat er sprake is van een slaapprobleem (reactief). Daarnaast is het mogelijk dat ouders die er zelf voor kiezen om samen in één bed te slapen, slaapproblemen over- of onderrapporteren, al naar gelang zij samen in één bed slapen als een probleem zien, of juist niet.
De auteurs stellen dat er zowel een behoorlijk aantal artikelen zijn die laten zien dat samen in één bed slapen geassocieerd is met meer slaapproblemen bij kinderen, maar dat er ook studies zijn die gemengde of niet eenduidige relaties lieten zien, en ook een behoorlijk aantal studies waarbij er geen relatie werd gevonden tussen samen in één bed slapen en slaapproblemen. Er werden slechts drie artikelen besproken waarin geconcludeerd wordt dat samen in één bed slapen geassocieerd is met minder slaapproblemen.
Er is weinig literatuur over de relatie tussen samen in één bed slapen en het ontwikkelen van autonomie.[218] De twee gevonden artikelen laten gemengd bewijs zien. Over gehechtheid concluderen de auteurs dat de relatie tussen samen in één bed slapen en gehechtheid nooit direct werd getest. In een ander recent onderzoek onder 550 moeders van baby’s bleek dat alleen slapen (nooit in één bed) versus samen in één bed slapen (altijd, en af en toe), het relatieve risico op de classificatie onveilig gehechtheid voor alleen slapende kinderen verhoogde.[204] Er was echter geen sprake van een dosis-respons relatie tussen samen slapen en gehechtheid als samen slapen in drie categorieën werd verdeeld (altijd samen slapen, af en toe samen slapen en altijd alleen slapen). Er was geen data beschikbaar over ouders en baby’s die samen in één kamer sliepen (die werden onder de alleen slapers geteld). Ouders die samen in één bed met hun kind sliepen, deden vaker aan proximale nachtelijke troosttechnieken (dicht bij het lichaam houden). Echter, nachtelijke troosttechnieken waren niet significant geassocieerd met veilige of gedesoriënteerde gehechtheid op de leeftijd van 14 maanden.
Als ouders zelf toch voor dit alternatief kiezen, is het uiteraard belangrijk om ouders volgens de JGZ-richtlijn Preventie wiegendood te adviseren hoe zij op een veilige manier samen kunnen slapen.
Naast het onderzoek naar samen in één bed slapen, zijn er een aantal onderzoeken gedaan naar samen met de baby op de kamer slapen, waarbij geen verschil wordt gemaakt tussen samen in één bed slapen, of in een eigen babybed op dezelfde kamer van de ouders. In een studie naar 153 families bleek dat moeders van baby’s die samen sliepen vaker ’s nachts wakker worden rapporteerden, dan moeders van baby’s die alleen op een kamer sliepen.[219] Echter, geen enkele objectieve slaapmaat was significant verschillend tussen samen-slapers en alleen-slapers, nadat er gecorrigeerd werd voor (borst)voeding. Samen slapende moeders hadden significant vaker objectieve en subjectieve slaapverstoringen dan moeders in de alleen-slapende groep. Slechtere slaap gedurende de zwangerschap en bij drie maanden voorspelde hogere niveaus van samen slapen op 6 maanden.
Samen slapen en cortisolniveaus
Uit onderzoek onder Nederlandse baby’s van 5 weken oud die alleen sliepen (alleen op een kamer), bleek dat zij een verhoogde cortisolniveau-reactie nadat zij uit bad werden gehaald, in vergelijking tot baby’s die frequent samen sliepen (in bed bij de moeder, of in een eigen babybed in de kamer van de moeder).[220] In datzelfde onderzoek werd geen effect gevonden van samen slapen (in bed bij de moeder, of in een eigen babybed in de kamer van de moeder) op de cortisolniveau-reactie na het krijgen van een vaccinatie op de leeftijd van 2 maanden.
In een ander onderzoek bleek dat op de leeftijd van 12 maanden, na het controleren voor o.a. de sensitiviteit van de moeder, gehechtheidsstatus en (borst)voeding, aantal weken waarbij er samen geslapen werd (in het bed van de moeder, of in een eigen bed op de kamer van de moeder) een lagere cortisolniveau reactiviteit voorspelde na de “onbekende situatie” procedure.[221]
In een ander onderzoek werd op basis van retrospectieve data over samen slapen (zowel in bed met ouders als in dezelfde kamer) geconcludeerd dat kinderen die samen met ouders in een kamer of in bed hadden geslapen, lagere cortisolniveaus hadden.[222]
Bovenstaande drie onderzoeken wijzen in de richting dat samen slapen gerelateerd is aan lagere cortisolniveaus of cortisolniveau-reactiviteit. In tegenstelling tot deze studies werd in een andere studie onder 92 families gevonden dat zowel samen slapen (in bed bij de ouders of in dezelfde kamer) en vaker ‘s nachts wakker worden wel geassocieerd waren met een verhoogde cortisolniveau-reactiviteit na vaccinatie op de leeftijd van 6 maanden en 12 maanden.[223] ‘s Nachts wakker worden op de leeftijd van 6 maanden was ook geassocieerd met een kleine verhoogde cortisol reactie na vaccinatie bij 12 maanden. De resultaten die gericht waren op het onderzoeken van de richting van de invloed suggereren dat samen slapen en ’s nachts wakker worden eerder de stressreactie beïnvloeden, dan andersom.
Conclusie
Er is behoefte aan meer onderzoek naar alternatieve interventies voor het verminderen van slaapproblemen bij jonge kinderen. Alternatieve interventies bestaan, maar veel zijn ofwel nog niet onderzocht, ofwel blijken niet effectief. Bijvoorbeeld samen in één bed slapen, wat soms aan ouders wordt geadviseerd als sensitieve en responsieve oplossing voor het slaapprobleem, lijkt vaker samen te gaan met meer slaapproblemen dan met minder slaapproblemen. Bovendien zijn er inconsistente resultaten wat betreft cortisolniveaus bij kinderen die samen slapen en in de meeste onderzoeken worden de categorieën samen in één bed slapen en samen in dezelfde kamer slapen niet apart geanalyseerd. Als ouders voor dit alternatief kiezen, is het uiteraard belangrijk om ouders volgens de JGZ-richtlijn Preventie Wiegendood te adviseren hoe zij op een veilige manier samen kunnen slapen; dit kan op zijn vroegst pas na de leeftijd van 4 maanden.
6.4.5 Algemene conclusie
De wetenschappelijke evidentie rond slapen, uitdoving, sensitief en responsief opvoeden, cortisol en gehechtheid is, als er al onderzoek beschikbaar is, over het algemeen van matige methodologische kwaliteit en oorzakelijke relaties zijn nauwelijks aangetoond. Het is belangrijk dat er meer robuust onderzoek wordt gedaan. Voor de professional is het aan te bevelen de wetenschappelijke literatuur rond dit thema bij te houden en kritisch te analyseren.
Op basis van bovenstaande beschikbare onderzoeken heeft de werkgroep geconcludeerd dat het toepassen van uitdoving bij bestaande slaapproblemen bij kinderen vanaf ongeveer 6 maanden effectief en veilig is. Een sensitieve en responsieve opvoeding sluit uitdoving niet uit. In de meeste gevallen is uitdoving binnen een paar dagen effectief en kunnen ouders de moeilijke en stressvolle periode tijdens het slaapprobleem doorbreken. Bovendien ontbreekt het op dit moment aan bewezen effectieve alternatieve interventies. Uiteraard moet met ouders worden overlegd welke interventie hun voorkeur heeft en moeten zij adequaat ondersteund worden, omdat het toepassen van deze interventies veel doorzettingsvermogen vergt van ouders.
6.5 Melatonine en andere Geneesmiddelen
6.5.1 Melatonine
Melatonine is een vetoplosbaar neurohormoon dat geproduceerd wordt in het corpus pineale (epifyse). De melatonineproductie is gekoppeld aan het circadiane ritme van de biologische klok. Het klokritme wordt beïnvloedt door licht wat op de retina valt (zie sectie Definities en achtergrondinformatie bij slaapritme). In de baarmoeder produceert de foetus zelf nog geen melatonine, maar ontvangt het via de placenta melatonine wat door de moeder geproduceerd wordt. Na de geboorte verdwijnt de door de moeder geproduceerde melatonine snel. Gedurende de eerste 3 levensmaanden lijkt melatonine afwezig, daarna start de productie langzaam op tot er een maximum wordt bereikt tussen de 1 tot 3 jarige leeftijd.
Bijwerkingen
Er lijken geen ernstige of schadelijke bijwerkingen te zijn van melatoninegebruik bij kinderen. De meest voorkomende bijwerkingen die worden gerapporteerd zijn: slaperigheid in de ochtend, verhoogde kans op bedplassen, hoofdpijn, duizeligheid, diarree, huiduitslag, en hypothermie. Lichte voorbijgaande hoofdpijn en gastro-intestinale symptomen worden voornamelijk gemeld tijdens de eerste dagen van de behandeling.
Lange termijn effecten
Melatonine wordt slecht enkele tientallen jaren toegepast, dus er is nog weinig bekend over lange termijn effecten of de interactie met de puberteitsontwikkeling.
Advisering en begeleiding binnen de JGZ
De aanbeveling voor JGZ professionals is om ouders in principe af te raden om melatonine te gebruiken en met een gedragsmatige aanpak te starten. Echter, melatonine is vrij verkrijgbaar en ouders of jongeren kunnen zelf gestart zijn met het innemen van melatonine. Volg in dat geval sectie Signalering, diagnostiek en verwijzen uit deze richtlijn, waaronder het hoofdstuk over het uitsluiten van een medische oorzaak van het slaapprobleem en slaapstoornissen en neem een uitgebreide anamnese af (zie Bijlage 1). Bespreek met ouders dat veel slaapproblemen meestal kunnen worden verholpen met een gedragsmatige aanpak (zie Thema 6. “Interventie en begeleiding bij slaapproblemen”).
JGZ professionals kunnen jeugdigen, waarbij mogelijk sprake is van een verstoorde biologische klok of waarbij een gedragsmatige aanpak niet effectief was, doorverwijzen naar een specialist in het ziekenhuis. Een specialist in het ziekenhuis kan een verstoorde biologische klok diagnosticeren. Hoewel JGZ professionals geen melatonine voorschrijven, volgt hieronder ter informatie een samenvatting van de Europese consensus-richtlijn voor melatoninegebruik bij kinderen.[180]
Samenvatting Europese consensus-richtlijn voor melatoninegebruik bij kinderen
Vertel ouders dat melatonine bij onjuist gebruik nadelige bijwerkingen kan hebben (zoals het verergeren van het slaapprobleem, invloed op prestaties overdag en medicatieafhankelijkheid), bij correct gebruik is melatonine in principe wel veilig (vanaf 6 maanden).
Adviseer dat melatonine alleen ingezet kan worden bij jeugdigen die moeite hebben om in slaap te vallen en/of moeite hebben ‘s ochtends op tijd op te staan. Melatonine dient volgens de Europese consensus-richtlijn van Bruni en collega’s [180] alleen gebruikt te worden bij een slaap-waak ritmestoornis door een verstoorde biologische klok, wanneer een gedragsmatige aanpak met regulatie van het slaapwaakritme en lichttherapie geen effect hebben gehad. Melatonine is niet effectief bij doorslaapproblemen.
Bij inzet van melatonine om de “klok gelijk te zetten” (“chronobiotic”):
Tijdstip van inname:
Het optimale tijdstip van inname hangt samen met de eigen aanmaak van melatonine. Deze kan geschat worden op basis van anamnese en slaap-waak dagboek, of bepaald worden middels een de “Dim Light Melatonin Onset” (DLMO) meting. Afhankelijk van de beschikbare informatie is het optimale tijdstip van inname dan 2-3 uur voor de DLMO of 3-4 uur voor men normaal gesproken in slaap valt (dus niet 3-4 uur voordat men wil slapen).
Dosering:
Start met een lage dosering van 0,2- 0,5 mg “fast release” melatonine. Verhoog de dosering met 0,2-0,5 mg (tot een maximum van 3 mg, bij adolescenten 5 mg) elke week indien nodig, totdat het effect heeft. Als 1 mg effectief is, probeer dan de dosis te verminderen.
Maximale dosis: <40 Kg: 3 mg; >40 Kg: 5 mg. Verwijs ouders door naar een specialist in het ziekenhuis of een slaapcentrum als de dosis steeds verhoogd moet worden (vanaf 1,5 mg). Het is namelijk belangrijk om vast te stellen of er geen stapelingen in melatonine ontstaan, met als gevolg dat de behandeling met melatonine niet meer effectief is.
Duur van de behandeling:
De duur van de behandeling moet aansluiten bij de specifieke patiënt, en in verhouding zijn met bijvoorbeeld de neurologische ontwikkelingsachterstand, maar mag in ieder geval niet minder dan 1 maand duren. De behandeling kan worden stopgezet net voor de puberteit, of net na de puberteit, i.v.m. de normale ontwikkeling bij adolescenten waarbij de biologische klok verschuift (zie inleiding van de richtlijn). Het te vroeg stoppen van een succesvolle behandeling kan ervoor zorgen dat het slaapprobleem weer terugkomt. Stop gedurende een week met de behandeling met melatonine (bij voorkeur in de zomer), nadat een normale slaap-cyclus is bereikt, om na te gaan of melatoninegebruik nog steeds nodig is.
Als de behandeling niet (meer) werkt:
Verwijs door naar een kinderarts of specialist in een slaapcentrum.
Controleer het tijdstip van de toediening, misschien wordt het te laat ingenomen.
Let erop dat als de behandeling niet meer effectief lijkt, dat dit mogelijk verklaard kan worden door een langzaam melatonine metabolisme.
Comedicatie kan het melatonine metabolisme beïnvloeden. Een langzamer metabolisme kan veroorzaakt worden door: anticonceptie pil, cimetidine, fluvoxamine. Een sneller metabolisme kan veroorzaakt worden door: carbamazepine, esomeprazole, omeprazole.
In sommige gevallen moet de dosis worden verlaagd, in plaats van een escalatie van de dosis.
Als er doorslaapproblemen ontstaan tijdens de behandeling is de dosis waarschijnlijk te hoog.
6.5.2 Overige medicatie
Medicatie die wordt ingezet ter behandeling van bepaalde aandoeningen, kan zowel slaapverstoring veroorzaken als slaperigheid.
Aan medicatie gerelateerde slaperigheid komt voor bij tweede-generatie antipsychotica (ingezet ter behandeling van schizofrenie, bipolaire stoornis, en gedragsstoornissen).[181]
Antihistamines (Diphenhydramine, Hydroxyzine) hebben een slaapverwekkend effect hebben en kunnen dufheid overdag veroorzaken.[182]
Medicatie die wordt ingezet ter behandeling van ADHD heeft vaak ook als bijeffect dat het de slaap verstoort, bijvoorbeeld methylfenidaat (Ritalin) of atomoxetine.[183][184]
Bij langdurig gebruik van Synthetische Glucocorticoïden (Prednison of Dexamethason) komen slaapproblemen ook relatief vaak voor.[185]
Sommige medicijnen die worden ingezet bij de behandeling van bepaalde aandoeningen hebben juist een positief effect op de slaap. Zo hebben benzodiazepines het kenmerk op korte termijn de inslaapproblematiek te verminderen en de initiatie en behoud van non-REM slaap te bevorderen. Vanwege de spierverslappende eigenschappen wordt afgeraden deze medicatie te gebruiken bij een vermoeden van slaapapneu.[183]
Ook worden antidepressiva soms ingezet als behandeling voor slapeloosheid bij volwassenen. Ondanks het ontbreken van gegevens over toepassing bij kinderen worden antidepressiva met sederende effecten reeds vele jaren voorgeschreven om slapeloosheid bij kinderen te behandelen, vooral bij kinderen met een psychiatrische achtergrond. Echter kunnen sommige antidepressiva symptomen van het restless legs syndroom veroorzaken.[183]
Studies bij volwassenen laten zien dat gebruik van antipsychotica kan leiden tot een toegenomen slaapstadium 2 en delta slaap en een onderdrukking van de REM slaap.
Sommige anti-epileptica verminderen de mate van slaapfragmentatie en zorgen voor een stabilisatie van de slaap, terwijl andere anti-epileptica juist slaapstadium 1 en 2 verminderd en slow-wave slaap doet toenemen. Daarbij leidt veel anti-epileptica tot gewichtstoename, wat ook weer slaapapneu tot gevolg kan hebben.[183]
Bij medicatiegebruik is begeleiding door een arts essentieel.
6.5.3 Kruidensupplementen
Hoewel kruidensupplementen als algemeen veilig gelden voor toepassing door volwassenen, zijn ze nog niet goed getest bij kinderen. Studies bij volwassenen en één zeer kleine studie bij kinderen laten enige evidentie zien van valeriaanwortel in de behandeling van slapeloosheid.[152] Enige empirische data bestaat voor de sedatieve werking van hop. Kruidenpreparaten die samengesteld zijn uit limoenbalsem, kamille of passiebloem zijn niet of nauwelijks effectief en kava-kava en tryptophan zijn mogelijk gevaarlijk. Lavendel lijkt veilig wanneer toegepast als aromatherapie en kan mogelijk het nachtelijk ontwaken verminderen en afhankelijkheid van sederende medicatie voorkomen, hoewel hier geen systematisch onderzoek bij kinderen naar is uitgevoerd.[186]
7 Samenwerken en doorverwijzen
Een groot aantal zorgverleners en instanties heeft een taak bij het voorkomen, signaleren en behandelen van slaapproblemen en stoornissen. Hieronder wordt de taak van de JGZ geschetst en de taak van andere zorgverleners en instanties. Ook worden er aanbevelingen gedaan wat betreft de samenwerking daarin.
Aanbevelingen
7.1 Ketenpartners
Huisartsen
Soms raadplegen ouders de huisarts bij slaapproblemen.[18] Vanuit hun medische professie zijn de mogelijkheden van huisartsen om kinderen met slaapproblemen te begeleiden via een gedragsmatige aanpak beperkt. Wel kunnen huisartsen meedenken over een medische oorzaak en kennen zij vaak de context van het gezin. Daarnaast kunnen huisartsen doorverwijzen als zij zelf onvoldoende kennis en expertise hebben. Voor huisartsen is ten aanzien van volwassenen de NHG-Standaard Slaapproblemen en slaapmiddelen (tweede herziening) opgesteld. Deze standaard gaat niet over slaapproblemen bij kinderen.
Medewerkers voorschoolse voorzieningen (peuterspeelzalen, kinderopvang, gastouders) en leerkrachten
Pedagogisch medewerkers van peuterspeelzalen en kinderopvang en leerkrachten verkeren in een goede positie om vermoeidheid bij kinderen te signaleren. Pedagogisch medewerkers en leerkrachten zijn voor ouders een belangrijke gesprekspartner als het met hun kind niet goed gaat op de opvang of op school. Doel van een oudergesprek is meestal om meer inzicht te krijgen in de achtergronden van de gesignaleerde problemen, ervaringen uit te wisselen over hoe het kind zich op school en thuis gedraagt en afspraken te maken over de aanpak van het probleem. In overleg met de ouders, kunnen pedagogisch medewerkers en leerkrachten contact opnemen met de JGZ om de begeleiding en aanpak op elkaar af te stemmen. Bij meer complexe situaties kunnen de problemen van het kind ingebracht worden in de interne zorgstructuur op scholen, zoals het zorg- en adviesteam (ZAT), ondersteuningsteam van de school (OT) of bovenschools ondersteuningsteam (Blokland, 2010).
Ondersteuning bij slaapproblemen via internet
Online opvoedingsondersteuning verdient aparte vermelding. Het is een vorm van hulpverlening
waarbij ouders via internet informatie, advies of ondersteuning krijgen. ‘Digitale’ ondersteuning bij slaapproblemen is een vorm van online hulpverlening die door verschillende instellingen gegeven wordt. De laatste jaren verschijnen er steeds meer websites over slaapproblemen voor ouders, waarbij het streven is de betrouwbaarheid van de informatie te vergroten. JGZ professionals kunnen ouders wijzen op bruikbare en betrouwbare websites:
| Website | Informatie |
| www.opvoeden.nl | Informatie en advies voor ouders over slaap van kinderen van baby tot jong volwassene |
| www.cjg.nl | Informatie en advies voor ouders over slaap van kinderen van baby tot jong volwassene. |
| www.slimslapen.nl | Informatie en zelftest over slaap voor jongeren |
Slaapcentra
In Nederland is een aantal slaapcentra. In slaapcentra worden volwassenen en kinderen onderzocht en behandeld voor hun slaap- en/of waakstoornissen. Vaak is er een multidisciplinair behandelteam dat kan bestaan uit (kinder)neurologen, psychologen, psychiaters, fysiologen, orthopedagoog, kindergeneeskundigen, longgeneeskundigen, somnologen, etc. Om de slaapproblemen in kaart te brengen, beschikken slaapcentra over een breed pakket aan onderzoeksmethoden. Het behandelteam biedt vervolgens een behandeling aan die bij de patiënt past. Bij kinderen waar geen onderliggende lichamelijke problemen een rol spelen, bestaat de behandeling uit het veranderen van aangeleerd, voor slaap ongunstig, gedrag. Er kan cognitieve gedragstherapie worden toegepast waarbij kinderen leren ‘negatieve gedachten omtrent het slapen’ om te zetten in ‘positieve gedachten’ of in ‘slaap bevorderend gedrag’. Soms worden slaapproblemen van kinderen veroorzaakt door de interacties tussen ouders en hun kind. In dat geval wordt deze ouders pedagogische hulp aangeboden. Indien nodig wordt overlegd met verwijzers en andere kinderspecialisten.
Een specialist uit een ziekenhuis of een huisarts kan doorverwijzen naar een slaapcentrum. Een jeugdarts of verpleegkundig specialist kan rechtstreeks verwijzen. Meestal gebeurt dit als:
- De oorzaak van het slaapprobleem niet achterhaald kan worden
- Behandeling door een andere professional geen effect heeft
- Meerdere(medisch)specialismen nodig lijken voor de behandeling, bijvoorbeeld als er sprake is van een ontwikkelingsstoornis, leerstoornis, gedragsprobleem, of medische/psychiatrische aandoeningen, of bij psychiatrische problematiek bij ouders
- Er behoefte is aan een second opinion
Bezoek de website www.kindenslaap.com voor een actuele lijst van Slaap-waakcentra binnen Nederland.
| Multidisciplinaire poliklinieken voor slaapstoornissen bij kinderen | Website |
| Amsterdam slaapcentrum Slotervaart Ziekenhuis, Amsterdam |
www.slaapkliniek.nl |
| Centrum voor Slaap- en Waakstoornissen, Medisch Centrum Haaglanden, Den Haag | www.mchaaglanden.nl/stimulansz/ziekten-a-z/slaapproblemen-bij-kinderen |
| Slaapcentrum, Gelderse Vallei Ziekenhuis, Ede | http://www.geldersevallei.nl/informatie/1017/slaapproblemen-bij-kinderen-en-pubers |
| Slaapcentrum MST, Enschede | www.mst.nl |
| Centrum voor Slaapgeneeskunde Kempenhaeghe, Heeze | http://www.kempenhaeghe.nl/Epilepsie/440/5/496/0/0/Slaapcentrum/ |
| Centrum voor Slaapgeneeskunde ZGT, Hengelo/Almelo | https://www.zgt.nl/3714/centrum-voor-slaapgeneeskunde/ |
| Slaap-Waakcentrum SEIN, Zwolle | http://www.sein.nl/slaap-waakcentrum/ |
8 Totstandkoming richtlijn
8.1 Werkwijze
Bij de start van het project is een denktank, bestaande uit vertegenwoordigers van Jong Florence en GGD Haaglanden en richtlijnontwikkelaars van TNO, bij elkaar gekomen om overstijgend mee te denken over verschillende richtlijnen. In de eerste werkgroepvergadering (november 2014) zijn alle uitgangsvragen doorgenomen. Per uitgangsvraag is gekeken of deze samen kon gaan met een andere uitgangsvraag, welke in de inleiding beantwoord dienen te worden, welke artikelen en auteurs bij dat thema belangrijk zijn, welke vragen naast evidence based ook een practice based benadering verdienen, welke alleen practice based beantwoord kunnen worden en welke zoektermen in ieder geval gebruikt moesten worden. Daarnaast is er ook inhoudelijk gesproken over de uitgangsvragen. Hiermee waren de uitgangsvragen definitief vastgesteld. De richtlijn is ontwikkeld volgens de methode van evidence based richtlijnontwikkeling (EBRO) (CBO Kwaliteitsinstituut voor de Gezondheidszorg, 2007). De basis voor de richtlijn is een samenvatting van het beschikbare bewijs in de wetenschappelijke literatuur. Op basis hiervan zijn aanbevelingen geformuleerd voor de praktijk. De eerste versies van de richtlijn zijn besproken tijdens de werkgroepbijeenkomsten in maart en juni 2015. Tijdens deze bijeenkomsten werd de inhoud besproken en bediscussieerd.
In juni 2015 is de eerste conceptversie van de richtlijn voorgelegd aan de klankbordgroep. De commentaren zijn verwerkt en over details heeft nader overleg plaatsgevonden met enkele experts. In juli 2015 is de tweede conceptversie opgesteld. Deze is voorgelegd aan de RAC van het NCJ en ZonMw.
In september 2015 is in samenwerking met het NCJ het BDS protocol opgesteld. Naar aanleiding van de feedback op deze conceptversie is in november 2015 een derde conceptversie opgesteld voor de praktijktest en landelijke commentaarronde (november 2015 – februari 2016). De feedback die werd verzameld tijdens de praktijktest (zie rapportage[167]) en landelijke commentaarronde werd voorgelegd aan de werkgroep tijdens twee bijeenkomsten in april en mei 2016. Hierna is in juni 2016 een vierde conceptversie opgesteld die in een schriftelijke ronde is voorgelegd aan de werkgroep en de klankbordgroep. In augustus 2016 werd de vijfde conceptversie opgesteld die is voorgelegd aan de RAC van het NCJ en ZonMw.
In juni 2016 werden conceptindicatoren ontwikkeld. In juli 2016 werden de conceptindicatoren voorgelegd aan de indicatorenwerkgroep. In augustus 2016 werd een conceptrapport voor de indicatoren opgesteld.
In november 2016 werd het BDS protocol aangepast en voorgelegd aan de BDS redactieraad van het NCJ. Ook werd de richtlijn, naar aanleiding van de feedback van de RAC van het NCJ, aangepast en voorgelegd aan de werkgroep en enkele experts uit de klankbordgroep. De zesde conceptversie werd opgesteld en voorgelegd aan de RAC van het NCJ en ZonMw ter autorisatie.
8.2 Werkgroep en klankbordgroep
Bij de formatie van de werkgroep is gelet op een goede balans tussen wetenschappers, inhoudelijke experts en uitvoerende JGZ professionals.* De werkgroep bestond uit 12 personen:
Werkgroep
- Drs. Regine van Riemsdijk, afgevaardigde AJN , jeugdarts KNMG, werkzaam bij GGD Hart voor Brabant.
- Drs. Ellen Reurslag, jeugdarts GGD Zaanstreek Waterland.
- Karin Verheijen, jeugd/stafverpleegkundige JGZ Zuid Holland West
- Elly Driessen, afgevaardigde NVDA, doktersassistente bij de GGD Gelderland Zuid.
- Margreet de Ruiter, stafverpleegkundige JGZ (0-19 jaar) GGD Gelderland-Zuid en afgevaardigde V&V vakgroep Jeugd.
- Betty Bakker-Camu MSc, beleidsmedewerker/ projectleider bij Vitras/GGD Regio Utrecht, Klinisch Gezondheidswetenschapper afstudeerrichting verplegingswetenschap, expert op gebied van slaap en preventie slaapproblemen van jonge kinderen. Buitenpromovendus preventie van slaapproblemen bij jonge kinderen. Tevens vertegenwoordiger V&VN vakgroep Jeugd.
- Prof Frits Boer, emeritus hoogleraar kinder- en jeugdpsychiatrie AMC, specialist ontwikkelingspsychopathologie en slaapproblemen.
- Dr. Hans Hamburger, neuroloog, somnoloog, hoofd van het Amsterdam WaakSlaapCentrum en voorzitter van de Nederlandse vereniging voor Slaap- en Waak Onderzoek (NSWO).
- Dr. Kristiaan van der Heijden, universitair hoofddocent bij Universiteit Leiden, Voorzitter PR-commissie en bestuurslid bij de NSWO.
- Drs. Daniëlle Hendriks, orthopedagoog-generalist en somnoloog, MCH Westeinde, afdeling Centrum voor slaap- en waakstoornissen, afdeling kind.
- Marijke van Noort, lactatiekundige IBCLC, afgevaardigde Nederlandse vereniging lactatiekundigen (NVL).
- Edwin Bos, ouder.
Vanuit TNO zijn daar de volgende mensen bij aangesloten:
- Drs. Maaike Beltman, bioloog, onderzoeker/ projectleider en teamcoördinator bij TNO.
- Drs. Eline Vlasblom, onderzoeker, richtlijnontwikkelaar, slaapdeskundige.
- Dr. Bregje van Sleuwen, onderzoeker, richtlijnontwikkelaar, slaapdeskundige. Sinds 2016 werkzaam bij Bernhoven.
- Dr. Monique L’Hoir, onderzoeker, richtlijnontwikkelaar, slaapdeskundige. Sinds 2016 werkzaam bij GGD Noord- en Oost-Gelderland en Wageningen University & Research.
Klankbordgroep
- Dr. Ed de Bruin, Universiteit van Amsterdam, Onderzoeker, ontwikkelde een innovatief programma om jongeren met slaapklachten te behandelen.
- Drs. Zamire Damen-van Beek, huisarts, vertegenwoordiger NHG.
- Dr. Adele Engelberts, vertegenwoordiger NVK, kinderarts Zuyderland Ziekenhuis Sittard-Geleen.
- Dr. Sigrid Pillen, vertegenwoordiger NVK, kinderneuroloog Kempenhaeghe, expertisecentrum epileptologie, slaapgeneeskunde en neurologische leer- en ontwikkelingsstoornissen.
- Lianne Verstraten, stafverpleegkundige GGD Gelderland Midden.
- Marjolein Keij, vertegenwoordiger Pharos, jeugdverpleegkundige.
*Een afgevaardigde van het Nederlands Instituut van Psychologen (NIP) werd op het moment van het indienen van de aanvraag uitgenodigd voor de werkgroep en hier werd door het NIP gehoor aan gegeven. Het NIP heeft gedurende het project echter besloten niet langer mee te werken aan de richtlijn. Het NIP stelde dat “de inhoudelijk deskundige die vanuit het NIP (sectie Het Jonge Kind) heeft meegelezen constateert dat de concept-richtlijn onvoldoende rekening houdt met de huidige kennis en wetenschap over hechting, sensitief ouderschap, en wat normaal slaapgedrag is bij baby’s”.
De voorgestelde aanpassingen door het NIP werden door de werkgroep kritisch bekeken. Een aantal voorgestelde aanpassingen konden worden overgenomen. Naar aanleiding van deze discussie en omdat vanuit de praktijktest bleek dat er bij JGZ professionals behoefte was aan meer informatie over dit onderwerp werd de bijlage “Sensitief opvoeden en een kind dat niet slaapt” opgenomen in de richtlijn. Een afgevaardigde van de Nederlandse Vereniging voor Gezondheidszorgpsychologie is gevraagd de laatste conceptversie van de richtlijn te beoordelen. Deze afgevaardigde geeft aan dat er zorgvuldig is gekeken naar de effecten van (ongemodificeerde) uitdoving op hechtingsstijl van kinderen en onderschrijft daarmee de aanbevelingen in de richtlijn.
8.3 Belangenverstrengeling
Voor de ontwikkeling van deze richtlijn is financiering verkregen van ZorgOnderzoek
Nederland Medische Wetenschappen (ZonMw). Alle werkgroepleden hebben een verklaring belangenverstrengeling ingevuld.
Dr Hamburger geeft aan in de laatste drie jaar (tot op heden) wel een relatie of bemoeienis te hebben gehad met meerdere bedrijven (zie ismc.nl 2014) die op enigerlei wijze zijn verbonden aan het onderwerp van de onderhavige JGZ-richtlijn, waardoor een belangenconflict zou kunnen ontstaan met de werkzaamheden in de richtlijnwerkgroep.
Dr L’Hoir geeft aan in de laatste drie jaar (tot op heden) werkzaamheden te hebben uitgevoerd in de vorm van een publicatie van een boek over slaap en wiegendood preventie (zie Het Slaapboek, 2015).
Dr van Sleuwen geeft aan in de laatste drie jaar (tot op heden) werkzaamheden te hebben uitgevoerd in de vorm van een publicatie van een boek over slaap en wiegendood preventie (zie Het Slaapboek, 2015).
De overige werkgroepleden hebben verklaard in de laatste drie jaar (tot op heden) geen relatie of bemoeienis te hebben gehad met bedrijven of organisaties, zoals sponsors, farmaceutische industrie, belangenvereniging, of werkzaamheden te ontplooien vanuit een eigen bedrijf of (mede) methoden, instrumenten ed. te ontwikkelen op het gebied van slaap en/of slaapgedrag, waardoor een belangenconflict zou kunnen ontstaan met de werkzaamheden in de richtlijnwerkgroep.
8.4 Cliënten participatie
Bij de ontwikkeling van de richtlijn is rekening gehouden met het patiënten perspectief. Edwin Bos, ouder, heeft een actieve bijdrage geleverd aan de werkgroep.
Daarnaast zijn er twee focusgroepen uitgevoerd. Een focusgroep met ouders en een focusgroep met jongeren. In de rapportage van de praktijktest is een uitgebreid verslag van deze focusgroepen te vinden.[167]
9 Verantwoording
9.1 Wetenschappelijke bewijsvoering
Er werd systematisch literatuur gezocht bij de uitgangsvragen die naar mening van de RAC niet in de inleiding van de richtlijn beantwoord dienden te worden (zie Uitgangsvragen). Een uitzondering hierop werd gemaakt voor risico- en beschermende factoren, hiervoor werd wel systematisch naar literatuur gezocht. De uitgangsvragen waar een systematisch literatuur voor werd gezocht werden samengevoegd in vijf onderwerpen:
- Risico- en beschermende factoren,
- Samenhangende stoornissen en ontwikkelingsproblemen,
- Geneesmiddelen,
- Signaleren,
- Preventie en interventie.
De literatuursearch richtte zich in eerste instantie op meta-analyses en systematische reviews uit de periode 2005 tot en met 2014, omdat de literatuursearch zonder deze limitatie een onwerkbare hoeveelheid artikelen opleverde. Dit resulteerde in een lijst met 446 geselecteerde referenties.
Hieruit volgde een lijst met abstracts. De abstracts zijn door twee personen beoordeeld op relevantie voor het beantwoorden van de uitgangsvragen. Dit resulteerde in een lijst van 120 artikelen waarvan de volledige tekst werd opgevraagd en doorgenomen. Na het doorlezen van de volledige tekst bleken 95 artikelen relevant.
Voor enkele onderwerpen bleken er onvoldoende reviews of meta-analyses te zijn geïncludeerd via de zoekstrategie (bijv. over de relatie tussen alcohol, drugsgebruik, tijdstip van de start van de school en slaap, interventies bij kinderen en adolescenten), daarom werd per onderwerp gezocht naar aanvullende reviews, meta-analyses, of bij afwezigheid daarvan, RCT’s of andere empirische artikelen. Daarnaast werd aan deze lijst m.b.v. de sneeuwbalmethode artikelen en aanvullende aangedragen literatuur door werkgroepleden in totaal 165 artikelen toegevoegd.
De geselecteerde artikelen zijn beoordeeld op relevantie voor de uitgangsvraag en op hun methodologische kwaliteit volgens EBRO-methode (zie Tabel 1). Artikelen van matige of slechte kwaliteit werden uitgesloten. Na deze selectie bleven de artikelen over die als onderbouwing bij de verschillende conclusies in de richtlijn staan vermeld. De evidence is samengevat in ‘evidentietabellen’ (zie bijlage). De beoordeling van de verschillende artikelen staat in de verschillende hoofdstukken onder het kopje ‘onderbouwing’. De literatuur is samengevat in een conclusie, waarbij het niveau van het relevante bewijs is weergegeven. De formulering van de conclusie is rechtstreeks gekoppeld aan het niveau van het bewijs, eveneens volgens de EBRO methode (zie Tabel 2).
Tabel 1. Indeling van de methodologische kwaliteit van individuele studies (bron: CBO 2007)
| Interventie | Diagnostisch accuratesse onderzoek | Schade/bijwerkingen*, etiologie | |
| A1 | Systematische review van tenminste twee onafhankelijk van elkaar uitgevoerde onderzoeken van A2-niveau | ||
| A2 | Gerandomiseerd dubbelblind vergelijkend klinisch onderzoek van goede kwaliteit van voldoende omvang | Onderzoek ten opzichte van een referentietest (een ‘gouden standaard’) met tevoren gedefinieerde afkapwaarden en onafhankelijke beoordeling van de resultaten van test en gouden standaard, betreffende een voldoende grote serie van opeenvolgende patiënten die allen de index- en referentietest hebben gehad |
Prospectief cohort onderzoek van voldoende omvang en follow-up, waarbij adequaat gecontroleerd is voor ‘confounding’ en selectieve follow-up voldoende is uitgesloten. |
| B | Vergelijkend onderzoek, maar niet met alle kenmerken als genoemd onder A2 (hieronder valt ook patiënt-controle onderzoek, cohort-onderzoek) | Onderzoek ten opzichte van een referentietest, maar niet met alle kenmerken die onder A2 zijn genoemd | Prospectief cohort onderzoek, maar niet met alle kenmerken als genoemd onder A2 of retrospectief cohort onderzoek of patiënt-controle onderzoek |
| C | Niet-vergelijkend onderzoek | ||
| D | Mening van deskundigen | ||
Tabel 2. Indeling van het eindoordeel (conclusie) (bron: CBO 2007)
| Eindoordeel (conclusie) gebaseerd op: | |
| 1 | Onderzoek van niveau A1 of ten minste twee onafhankelijk van elkaar uitgevoerde onderzoeken van niveau A2. |
| 2 | Eén onderzoek van niveau A2 of ten minste twee onafhankelijk van elkaar uitgevoerde onderzoeken van niveau B. |
| 3 | Eén onderzoek van niveau B of C. |
| 4 | Mening van deskundigen. |
9.1.1 Knelpuntanalyse
Niet beschikbaar, deze richtlijn is in herziening.
9.1.2 Zoekstrategie
Gezocht is in Pubmed, PsycInfo, Cochrane en CINAHL. In Pubmed werd gezocht met behulp van MESHterms. De volgende zoektermen zijn gebruikt:
Pubmed, gezocht op 4-12-2014. In Pubmed werd gezocht met behulp van o.a. MESH terms.
| Onderwerp uitgangsvragen | Zoektermen |
| Risico- en beschermende factoren | (((((((((((“child”[Title/Abstract]) OR “infant”[Title/Abstract]) OR “preschool”[Title/Abstract]) OR “adolescent”[Title/Abstract]) OR “newborn”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR ((((“Child”[Mesh]) OR “Child, Preschool”[Mesh]) OR “Infant”[Mesh]) OR “Adolescent”[Mesh]))) AND ((((((((((((((((“sleep problems”[Title/Abstract]) OR “sleeping problems”[Title/Abstract]) OR “sleep patterns”[Title/Abstract]) OR “sleep quality”[Title/Abstract]) OR “sleep characteristics”[Title/Abstract]) OR “sleep behavior”[Title/Abstract]) OR “sleep duration”[Title/Abstract]) OR “sleeping patterns”[Title/Abstract]) OR “sleeping quality”[Title/Abstract]) OR “sleeping characteristics”[Title/Abstract]) OR “sleeping behavior”[Title/Abstract]) OR “sleeping duration”[Title/Abstract]))) OR ((((“sleep”[Title/Abstract]) OR “sleep deprivation”[Title/Abstract]) OR “sleep disorders”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR (((“Sleep”[Mesh]) OR “Sleep Deprivation”[Mesh]) OR “Sleep Disorders”[Mesh])))) AND (((((((((“protective factors”[Title/Abstract]) OR “enabling factors”[Title/Abstract]) OR “enhancing factors”[Title/Abstract]) OR “improving factors”[Title/Abstract]) OR “protecting factors”[Title/Abstract]) OR “inhibiting factors”[Title/Abstract])) OR ((((“risk factor”[Title/Abstract]) OR “causality”[Title/Abstract]) OR “precipitating factors”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR (((“Risk Factors”[Mesh]) OR “Causality”[Mesh]) OR “Precipitating Factors”[Mesh])) |
| Samenhangende stoornissen en ontwikkelingsproblemen | (((((((((((((((((((((((“comorbidity”[Title/Abstract]) OR “child development”[Title/Abstract]) OR “adolescent development”[Title/Abstract]) OR “mental disorders”[Title/Abstract]) OR “developmental disabilities”[Title/Abstract]) OR “child behavior”[Title/Abstract]) OR “adolescent behavior”[Title/Abstract]) OR “child behavior disorders”[Title/Abstract]) OR “apnea”[Title/Abstract]) OR “respiratory disorders”[Title/Abstract]) OR “reflux”[Title/Abstract]) OR “respiratory”[Title/Abstract]) OR “eczema”[Title/Abstract]) OR “overweight”[Title/Abstract]) OR “obesity”[Title/Abstract]) OR “vision disorders”[Title/Abstract]) OR “asthma”[Title/Abstract]) OR “growth”[Title/Abstract]) OR “melatonin”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR ((“Comorbidity”[Mesh]) OR (((((((((((((((((“Child Development”[Mesh]) OR “Adolescent Development”[Mesh]) OR “Mental Disorders Diagnosed in Childhood”[Mesh]) OR “Developmental Disabilities”[Mesh]) OR “Child Behavior”[Mesh]) OR “Adolescent Behavior”[Mesh]) OR “Child Behavior Disorders”[Mesh]) OR “Apnea”[Mesh]) OR “Respiration Disorders”[Mesh]) OR “Gastroesophageal Reflux”[Mesh]) OR “Signs and Symptoms, Respiratory”[Mesh]) OR “Skin Diseases, Eczematous”[Mesh]) OR “Body Weight”[Mesh]) OR “Vision Disorders”[Mesh]) OR “Asthma”[Mesh]) OR “Growth”[Mesh]) OR “Melatonin”[Mesh])))) AND ((((((((((“child”[Title/Abstract]) OR “infant”[Title/Abstract]) OR “preschool”[Title/Abstract]) OR “adolescent”[Title/Abstract]) OR “newborn”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR ((((“Child”[Mesh]) OR “Child, Preschool”[Mesh]) OR “Infant”[Mesh]) OR “Adolescent”[Mesh]))) AND ((((((((((((((((“sleep problems”[Title/Abstract]) OR “sleeping problems”[Title/Abstract]) OR “sleep patterns”[Title/Abstract]) OR “sleep quality”[Title/Abstract]) OR “sleep characteristics”[Title/Abstract]) OR “sleep behavior”[Title/Abstract]) OR “sleep duration”[Title/Abstract]) OR “sleeping patterns”[Title/Abstract]) OR “sleeping quality”[Title/Abstract]) OR “sleeping characteristics”[Title/Abstract]) OR “sleeping behavior”[Title/Abstract]) OR “sleeping duration”[Title/Abstract]))) OR ((((“sleep”[Title/Abstract]) OR “sleep deprivation”[Title/Abstract]) OR “sleep disorders”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR (((“Sleep”[Mesh]) OR “Sleep Deprivation”[Mesh]) OR “Sleep Disorders”[Mesh]))) |
| Geneesmiddelen | (((((((((((“pharmaceutical”[Title/Abstract]) OR “medication”[Title/Abstract]) OR “drug”[Title/Abstract]) OR “melatonin”[Title/Abstract]) OR “ritalin”[Title/Abstract]) OR “caffeine”[Title/Abstract]) OR “methylphenidate”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat])))) OR ((“Pharmaceutical Preparations”[Mesh]) OR (((“Melatonin”[Mesh]) OR “Caffeine”[Mesh]) OR “Methylphenidate”[Mesh]))) AND ((((((((((“child”[Title/Abstract]) OR “infant”[Title/Abstract]) OR “preschool”[Title/Abstract]) OR “adolescent”[Title/Abstract]) OR “newborn”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR ((((“Child”[Mesh]) OR “Child, Preschool”[Mesh]) OR “Infant”[Mesh]) OR “Adolescent”[Mesh]))) AND ((((((((((((((((“sleep problems”[Title/Abstract]) OR “sleeping problems”[Title/Abstract]) OR “sleep patterns”[Title/Abstract]) OR “sleep quality”[Title/Abstract]) OR “sleep characteristics”[Title/Abstract]) OR “sleep behavior”[Title/Abstract]) OR “sleep duration”[Title/Abstract]) OR “sleeping patterns”[Title/Abstract]) OR “sleeping quality”[Title/Abstract]) OR “sleeping characteristics”[Title/Abstract]) OR “sleeping behavior”[Title/Abstract]) OR “sleeping duration”[Title/Abstract]))) OR ((((“sleep”[Title/Abstract]) OR “sleep deprivation”[Title/Abstract]) OR “sleep disorders”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR (((“Sleep”[Mesh]) OR “Sleep Deprivation”[Mesh]) OR “Sleep Disorders”[Mesh]))) |
| Signaleren | (((((((“screening”[Title/Abstract]) OR “early detection”[Title/Abstract]) OR “diagnosis”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat])))) OR ((((((“Sleep/diagnosis”[Mesh]) OR “Sleep Deprivation/diagnosis”[Mesh]) OR “Sleep Disorders/diagnosis”[Mesh]))))) AND ((((((((((“child”[Title/Abstract]) OR “infant”[Title/Abstract]) OR “preschool”[Title/Abstract]) OR “adolescent”[Title/Abstract]) OR “newborn”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR ((((“Child”[Mesh]) OR “Child, Preschool”[Mesh]) OR “Infant”[Mesh]) OR “Adolescent”[Mesh]))) AND ((((((((((((((((“sleep problems”[Title/Abstract]) OR “sleeping problems”[Title/Abstract]) OR “sleep patterns”[Title/Abstract]) OR “sleep quality”[Title/Abstract]) OR “sleep characteristics”[Title/Abstract]) OR “sleep behavior”[Title/Abstract]) OR “sleep duration”[Title/Abstract]) OR “sleeping patterns”[Title/Abstract]) OR “sleeping quality”[Title/Abstract]) OR “sleeping characteristics”[Title/Abstract]) OR “sleeping behavior”[Title/Abstract]) OR “sleeping duration”[Title/Abstract]))) OR ((((“sleep”[Title/Abstract]) OR “sleep deprivation”[Title/Abstract]) OR “sleep disorders”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR (((“Sleep”[Mesh]) OR “Sleep Deprivation”[Mesh]) OR “Sleep Disorders”[Mesh]))) |
| Preventie en interventie | ((((((((“prevention”[Title/Abstract]) OR “intervention”[Title/Abstract]) OR “therapy”[Title/Abstract]) OR “education”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR (((((((((“Sleep Deprivation/diet therapy”[Mesh] OR “Sleep Deprivation/drug therapy”[Mesh] OR “Sleep Deprivation/prevention and control”[Mesh] OR “Sleep Deprivation/therapy”[Mesh])) OR (“Adolescent/drug therapy”[Mesh] OR “Adolescent/therapy”[Mesh])) OR (“Child/drug therapy”[Mesh] OR “Child/prevention and control”[Mesh] OR “Child/therapy”[Mesh])) OR (“Child, Preschool/drug therapy”[Mesh] OR “Child, Preschool/therapy”[Mesh])) OR (“Infant/drug therapy”[Mesh] OR “Infant/prevention and control”[Mesh] OR “Infant/therapy”[Mesh]))) OR ((((“Sleep Initiation and Maintenance Disorders/diet therapy”[Mesh] OR “Sleep Initiation and Maintenance Disorders/drug therapy”[Mesh] OR “Sleep Initiation and Maintenance Disorders/prevention and control”[Mesh] OR “Sleep Initiation and Maintenance Disorders/therapy”[Mesh])) OR (“Sleep Disorders/diet therapy”[Mesh] OR “Sleep Disorders/drug therapy”[Mesh] OR “Sleep Disorders/prevention and control”[Mesh] OR “Sleep Disorders/therapy”[Mesh])) OR (“Sleep/diet therapy”[Mesh] OR “Sleep/drug therapy”[Mesh] OR “Sleep/prevention and control”[Mesh] OR “Sleep/therapy”[Mesh]))) OR (((((((“Pediatric Nursing/education”[Mesh]) OR “Nurse Practitioners/education”[Mesh]) OR “Parents/education”[Mesh]) OR “Child/education”[Mesh]) OR “Child, Preschool/education”[Mesh]) OR “Adolescent/education”[Mesh]) OR “Behavior Therapy”[Mesh])))) AND ((((((((((“child”[Title/Abstract]) OR “infant”[Title/Abstract]) OR “preschool”[Title/Abstract]) OR “adolescent”[Title/Abstract]) OR “newborn”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR ((((“Child”[Mesh]) OR “Child, Preschool”[Mesh]) OR “Infant”[Mesh]) OR “Adolescent”[Mesh]))) AND ((((((((((((((((“sleep problems”[Title/Abstract]) OR “sleeping problems”[Title/Abstract]) OR “sleep patterns”[Title/Abstract]) OR “sleep quality”[Title/Abstract]) OR “sleep characteristics”[Title/Abstract]) OR “sleep behavior”[Title/Abstract]) OR “sleep duration”[Title/Abstract]) OR “sleeping patterns”[Title/Abstract]) OR “sleeping quality”[Title/Abstract]) OR “sleeping characteristics”[Title/Abstract]) OR “sleeping behavior”[Title/Abstract]) OR “sleeping duration”[Title/Abstract]))) OR ((((“sleep”[Title/Abstract]) OR “sleep deprivation”[Title/Abstract]) OR “sleep disorders”[Title/Abstract]) AND (“2011/01/01″[PDat] : “3000/12/31″[PDat]))) OR (((“Sleep”[Mesh]) OR “Sleep Deprivation”[Mesh]) OR “Sleep Disorders”[Mesh]))) |
Psychinfo, gezocht op 4-12-2014
| Onderwerp uitgangsvragen | Zoektermen |
| Risico- en beschermende factoren | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“protective factor*” or “enabling factor*” or “enhancing factor*” or “improving factor*” or “protecting factor*” or “inhibiting factor*” or “risk factor*” or “causality” or “precipitating factor*”).ab,ti.) |
| Samenhangende stoornissen en ontwikkelingsproblemen | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“comorbid*” or “child development*” or “adolescent development*” or “mental disorder*” or “developmental disabilit*” or “child behavior*r*” or “adolescent behavior*r*” or “child behavior*r disorder*” or “apnea” or “respiratory disorder*” or “reflux” or “respiratory” or “eczema” or “overweight” or “obesity” or “vision disorder*” or “asthma” or “growth” or “melatonin”).ab,ti.) |
| Geneesmiddelen | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“pharmaceutical” or “medica*” or “drug*” or “melatonin” or “ritalin” or “caffeine” or “methylphenidate”).ab,ti.) |
| Signaleren | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“screen*” or “early detection” or “diagnos*”).ab,ti.) |
| Preventie en interventie | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“preventi*” or “intervention” or “therap*” or “education*”).ab,ti.) |
Cochrane, gezocht op 4-12-2014
Omdat de search bij Cochrane niet veel literatuur opleverde, werd de search bij Cochrane niet onderverdeeld in onderwerpen, maar werd breder gezocht naar: (child or children or infant* or newborn* or preschool* or adolescent*) AND sleep*
CINAHL, gezocht op 20-3-2015
| Onderwerp uitgangsvragen | Zoektermen |
| Risico- en beschermende factoren | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“protective factor*” or “enabling factor*” or “enhancing factor*” or “improving factor*” or “protecting factor*” or “inhibiting factor*” or “risk factor*” or “causality” or “precipitating factor*”).ab,ti.) |
| Samenhangende stoornissen en ontwikkelingsproblemen | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“comorbid*” or “child development*” or “adolescent development*” or “mental disorder*” or “developmental disabilit*” or “child behavior*r*” or “adolescent behavior*r*” or “child behavior*r disorder*” or “apnea” or “respiratory disorder*” or “reflux” or “respiratory” or “eczema” or “overweight” or “obesity” or “vision disorder*” or “asthma” or “growth” or “melatonin”).ab,ti.) |
| Geneesmiddelen | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“pharmaceutical” or “medica*” or “drug*” or “melatonin” or “ritalin” or “caffeine” or “methylphenidate”).ab,ti.) |
| Signaleren | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“screen*” or “early detection” or “diagnos*”).ab,ti.) |
| Preventie en interventie | ((child or children or infant* or newborn* or preschool* or adolescent*).ab,ti.) AND ((sleep*).ab,ti.) AND ((“preventi*” or “intervention” or “therap*” or “education*”).ab,ti.) |
9.1.3 Evidentietabellen en niveau van bewijsvoering
Zie Bestanden
9.2 Kennislacunes
- Er zijn geen cijfers bekend over de prevalentie van slaapproblemen bij Nederlandse adolescenten.
- Er is onvoldoende onderzoek gedaan naar cultuurverschillen in slaap binnen Nederland.
- Er is geen Nederlands onderzoek gedaan naar het effect van preventie van slaapproblemen bij kinderen ouder dan 18 maanden.
- Er is meer onderzoek nodig op welke manier voorlichting over slaap aansluit bij ouders met verschillende culturele achtergronden en lage gezondheidsvaardigheden.
- Er zijn onvoldoende in Nederland effectief bewezen interventies voor de behandeling van slaapproblemen bij kinderen tot 12 jaar.
Referenties
[1] Paruthi S, Brooks LJ, D'Ambrosio C, Hall WA, Kotagal S, Lloyd RM, Malow BA, Maski K, Nichols C, Quan SF, Rosen CL, Troester MM, Wise MS. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2016;12(6):785-6
http://dx.doi.org/10.5664/jcsm.5866 https://pubmed.ncbi.nlm.nih.gov/27250809[2] Boer F. Slaapproblemen bij kinderen: Kinderpsychologie in de praktijk Lannoo-Meulenhoff Belgium 2013
[3] Galland BC, Taylor BJ, Elder DE, Herbison P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep medicine reviews 2012;16(3):213-22
http://dx.doi.org/10.1016/j.smrv.2011.06.001 https://pubmed.ncbi.nlm.nih.gov/21784676[4] Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 2003;111(2):302-7
https://pubmed.ncbi.nlm.nih.gov/12563055[5] Meijer AM, van den Wittenboer GLH. Contribution of infants' sleep and crying to marital relationship of first-time parent couples in the 1st year after childbirth. Journal of family psychology : JFP : journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2007;21(1):49-57
https://pubmed.ncbi.nlm.nih.gov/17371109[6] Henderson JMT, France KG, Owens JL, Blampied NM. Sleeping through the night: the consolidation of self-regulated sleep across the first year of life. Pediatrics 2010;126(5):e1081-7
http://dx.doi.org/10.1542/peds.2010-0976 https://pubmed.ncbi.nlm.nih.gov/20974775[7] van Litsenburg RRL, Waumans RC, van den Berg G, Gemke RJBJ. Sleep habits and sleep disturbances in Dutch children: a population-based study. European journal of pediatrics 2010;169(8):1009-15
http://dx.doi.org/10.1007/s00431-010-1169-8 https://pubmed.ncbi.nlm.nih.gov/20191392[8] van der Heijden KB, de Sonneville LMJ, Swaab H. Association of eveningness with problem behavior in children: a mediating role of impaired sleep. Chronobiology international 2013;30(7):919-29
http://dx.doi.org/10.3109/07420528.2013.790041 https://pubmed.ncbi.nlm.nih.gov/23802509[9] Owens JA, Belon K, Moss P. Impact of delaying school start time on adolescent sleep, mood, and behavior. Archives of pediatrics & adolescent medicine 2010;164(7):608-14
http://dx.doi.org/10.1001/archpediatrics.2010.96 https://pubmed.ncbi.nlm.nih.gov/20603459[10] Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep medicine 2011;12(2):110-8
http://dx.doi.org/10.1016/j.sleep.2010.11.008 https://pubmed.ncbi.nlm.nih.gov/21257344[11] American Academy of Sleep Medicine. International classification of sleep disorders—third edition (ICSD-3) AASM Resource Library [online] 2014
[12] American Psychiatric Association. Diagnostic and statistical manual of mental disorders 5th ed. 2013
[13] American Academy of Sleep Medicine. International classification of sleep disorders. 2nd ed. Westchester, IL 2005
[14] Jenni OG, Fuhrer HZ, Iglowstein I, Molinari L, Largo RH. A longitudinal study of bed sharing and sleep problems among Swiss children in the first 10 years of life. Pediatrics 2005;115(1 Suppl):233-40
https://pubmed.ncbi.nlm.nih.gov/15866857[15] Byars KC, Yolton K, Rausch J, Lanphear B, Beebe DW. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics 2012;129(2):e276-84
http://dx.doi.org/10.1542/peds.2011-0372 https://pubmed.ncbi.nlm.nih.gov/22218837[16] Meltzer LJ, Plaufcan MR, Thomas JH, Mindell JA. Sleep problems and sleep disorders in pediatric primary care: treatment recommendations, persistence, and health care utilization. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2014;10(4):421-6
http://dx.doi.org/10.5664/jcsm.3620 https://pubmed.ncbi.nlm.nih.gov/24733988[17] van Sleuwen BE, Vlasblom E, L'Hoir MP. Eindverslag laagdrempelige verpleegkundige interventiemethoden in de jeugdgezondheidszorg bij slaapproblemen van jonge kinderen. ZonMW 2013
http://www.zonmw.nl/nl/projecten/project-detail/laagdrempelige-verpleegkundige-interventiemethoden-in-de-jeugdgezondheidszorg-bij-slaapproblemen-van/voortgang/[18] Linden M, Suijlekom-Smit L, Schellevis FG, Wouden J. Tweede nationale studie naar ziekten en verrichtingen in de huisartspraktijk. het kind in de huisartspraktijk. Utrecht: Nivel 2005
[19] Yperen T, Stam PT. Opvoeden versterken. Den Haag: VNG 2010
[20] Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A, . Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep 2006;29(10):1263-76
https://pubmed.ncbi.nlm.nih.gov/17068979[21] Ednick M, Cohen AP, McPhail GL, Beebe D, Simakajornboon N, Amin RS. A review of the effects of sleep during the first year of life on cognitive, psychomotor, and temperament development. Sleep 2009;32(11):1449-58
https://pubmed.ncbi.nlm.nih.gov/19928384[22] Hemmi MH, Wolke D, Schneider S. Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioural outcomes in childhood: a meta-analysis. Archives of disease in childhood 2011;96(7):622-9
http://dx.doi.org/10.1136/adc.2010.191312 https://pubmed.ncbi.nlm.nih.gov/21508059[23] Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK. Acute sleep restriction effects on emotion responses in 30- to 36-month-old children. Journal of sleep research 2012;21(3):235-46
http://dx.doi.org/10.1111/j.1365-2869.2011.00962.x https://pubmed.ncbi.nlm.nih.gov/21988087[24] Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep medicine reviews 2010;14(3):179-89
http://dx.doi.org/10.1016/j.smrv.2009.10.004 https://pubmed.ncbi.nlm.nih.gov/20093054[25] Koulouglioti C, Cole R, Kitzman H. Inadequate sleep and unintentional injuries in young children. Public health nursing (Boston, Mass.) 2008;25(2):106-14
http://dx.doi.org/10.1111/j.1525-1446.2008.00687.x https://pubmed.ncbi.nlm.nih.gov/18294179[26] Gregory AM, Van der Ende J, Willis TA, Verhulst FC. Parent-reported sleep problems during development and self-reported anxiety/depression, attention problems, and aggressive behavior later in life. Archives of pediatrics & adolescent medicine 2008;162(4):330-5
http://dx.doi.org/10.1001/archpedi.162.4.330 https://pubmed.ncbi.nlm.nih.gov/18391141[27] Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van Lenthe FJ, Brug J. Early-life determinants of overweight and obesity: a review of systematic reviews. Obesity reviews : an official journal of the International Association for the Study of Obesity 2010;11(10):695-708
http://dx.doi.org/10.1111/j.1467-789X.2010.00735.x https://pubmed.ncbi.nlm.nih.gov/20331509[28] Astill RG, Van der Heijden KB, Van Ijzendoorn MH, Van Someren EJW. Sleep, cognition, and behavioral problems in school-age children: a century of research meta-analyzed. Psychological bulletin 2012;138(6):1109-38
http://dx.doi.org/10.1037/a0028204 https://pubmed.ncbi.nlm.nih.gov/22545685[29] Owens J, Gruber R, Brown T, Corkum P, Cortese S, O'Brien L, Stein M, Weiss M. Future research directions in sleep and ADHD: report of a consensus working group. Journal of attention disorders 2013;17(7):550-64
http://dx.doi.org/10.1177/1087054712457992 https://pubmed.ncbi.nlm.nih.gov/22982880[30] Kheirandish L, Gozal D. Neurocognitive dysfunction in children with sleep disorders. Developmental science 2006;9(4):388-99
https://pubmed.ncbi.nlm.nih.gov/16764612[31] Nielsen LS, Danielsen KV, Sørensen TIA. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obesity reviews : an official journal of the International Association for the Study of Obesity 2011;12(2):78-92
http://dx.doi.org/10.1111/j.1467-789X.2010.00724.x https://pubmed.ncbi.nlm.nih.gov/20345429[32] Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep medicine reviews 2014;18(1):75-87
http://dx.doi.org/10.1016/j.smrv.2013.03.005 https://pubmed.ncbi.nlm.nih.gov/23806891[33] Moore M, Meltzer LJ. The sleepy adolescent: causes and consequences of sleepiness in teens. Paediatric respiratory reviews 2008;9(2):114-20; quiz 120-1
http://dx.doi.org/10.1016/j.prrv.2008.01.001 https://pubmed.ncbi.nlm.nih.gov/18513671[34] Vallido T, Peters K, O'Brien L, Jackson D. Sleep in adolescence: a review of issues for nursing practice. Journal of clinical nursing 2009;18(13):1819-26
http://dx.doi.org/10.1111/j.1365-2702.2009.02812.x https://pubmed.ncbi.nlm.nih.gov/19638045[35] de Bruin EJ, van Run C, Staaks J, Meijer AM. Effects of sleep manipulation on cognitive functioning of adolescents: A systematic review. Sleep medicine reviews 2017;32():45-57
http://dx.doi.org/10.1016/j.smrv.2016.02.006 https://pubmed.ncbi.nlm.nih.gov/27039223[36] Rutters F, Gerver WJ, Nieuwenhuizen AG, Verhoef SPM, Westerterp-Plantenga MS. Sleep duration and body-weight development during puberty in a Dutch children cohort. International journal of obesity (2005) 2010;34(10):1508-14
http://dx.doi.org/10.1038/ijo.2010.161 https://pubmed.ncbi.nlm.nih.gov/20714331[37] Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Association of short and long sleep durations with insulin sensitivity in adolescents. The Journal of pediatrics 2011;158(4):617-23
http://dx.doi.org/10.1016/j.jpeds.2010.09.080 https://pubmed.ncbi.nlm.nih.gov/21146189[38] Faraut B, Boudjeltia KZ, Vanhamme L, Kerkhofs M. Immune, inflammatory and cardiovascular consequences of sleep restriction and recovery. Sleep medicine reviews 2012;16(2):137-49
http://dx.doi.org/10.1016/j.smrv.2011.05.001 https://pubmed.ncbi.nlm.nih.gov/21835655[39] Orzech KM, Acebo C, Seifer R, Barker D, Carskadon MA. Sleep patterns are associated with common illness in adolescents. Journal of sleep research 2014;23(2):133-42
http://dx.doi.org/10.1111/jsr.12096 https://pubmed.ncbi.nlm.nih.gov/24134661[40] Mindell JA, Telofski LS, Wiegand B, Kurtz ES. A nightly bedtime routine: impact on sleep in young children and maternal mood. Sleep 2009;32(5):599-606
https://pubmed.ncbi.nlm.nih.gov/19480226[41] Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep medicine reviews 2010;14(2):89-96
http://dx.doi.org/10.1016/j.smrv.2009.05.003 https://pubmed.ncbi.nlm.nih.gov/19631566[42] Martin J, Hiscock H, Hardy P, Davey B, Wake M. Adverse associations of infant and child sleep problems and parent health: an Australian population study. Pediatrics 2007;119(5):947-55
https://pubmed.ncbi.nlm.nih.gov/17473096[43] Hunter LP, Rychnovsky JD, Yount SM. A selective review of maternal sleep characteristics in the postpartum period. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN 2009;38(1):60-8
http://dx.doi.org/10.1111/j.1552-6909.2008.00309.x https://pubmed.ncbi.nlm.nih.gov/19208049[44] Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep medicine 2009;10(7):771-9
http://dx.doi.org/10.1016/j.sleep.2008.07.016 https://pubmed.ncbi.nlm.nih.gov/19285450[45] Semple A. What influences baby-sleeping behaviour at night (1)? The practising midwife 2010;13(9):17-20
https://pubmed.ncbi.nlm.nih.gov/21138130[46] Malone SK. Early to bed, early to rise?: an exploration of adolescent sleep hygiene practices. The Journal of school nursing : the official publication of the National Association of School Nurses 2011;27(5):348-54
http://dx.doi.org/10.1177/1059840511410434 https://pubmed.ncbi.nlm.nih.gov/21606219[47] de Bruin EJ, van Kampen RKA, van Kooten T, Meijer AM. Psychometric properties and clinical relevance of the adolescent sleep hygiene scale in Dutch adolescents. Sleep medicine 2014;15(7):789-97
http://dx.doi.org/10.1016/j.sleep.2014.03.015 https://pubmed.ncbi.nlm.nih.gov/24891082[48] Galbally M, Lewis AJ, McEgan K, Scalzo K, Islam FA. Breastfeeding and infant sleep patterns: an Australian population study. Journal of paediatrics and child health 2013;49(2):E147-52
http://dx.doi.org/10.1111/jpc.12089 https://pubmed.ncbi.nlm.nih.gov/23331519[49] Ramamurthy MB, Sekartini R, Ruangdaraganon N, Huynh DHT, Sadeh A, Mindell JA. Effect of current breastfeeding on sleep patterns in infants from Asia-Pacific region. Journal of paediatrics and child health 2012;48(8):669-74
http://dx.doi.org/10.1111/j.1440-1754.2012.02453.x https://pubmed.ncbi.nlm.nih.gov/22616943[50] Rosen LA. Infant sleep and feeding. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN 2008;37(6):706-14
http://dx.doi.org/10.1111/j.1552-6909.2008.00299.x https://pubmed.ncbi.nlm.nih.gov/19012721[51] Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breastfeeding medicine : the official journal of the Academy of Breastfeeding Medicine 2015;10(5):246-52
http://dx.doi.org/10.1089/bfm.2014.0153 https://pubmed.ncbi.nlm.nih.gov/25973527[52] Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep medicine 2010;11(8):735-42
http://dx.doi.org/10.1016/j.sleep.2010.02.006 https://pubmed.ncbi.nlm.nih.gov/20673649[53] Vijakkhana N, Wilaisakditipakorn T, Ruedeekhajorn K, Pruksananonda C, Chonchaiya W. Evening media exposure reduces night-time sleep. Acta paediatrica (Oslo, Norway : 1992) 2015;104(3):306-12
http://dx.doi.org/10.1111/apa.12904 https://pubmed.ncbi.nlm.nih.gov/25521612[54] Falbe J, Davison KK, Franckle RL, Ganter C, Gortmaker SL, Smith L, Land T, Taveras EM. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 2015;135(2):e367-75
http://dx.doi.org/10.1542/peds.2014-2306 https://pubmed.ncbi.nlm.nih.gov/25560435[55] Owens JA, Mindell J, Baylor A. Effect of energy drink and caffeinated beverage consumption on sleep, mood, and performance in children and adolescents. Nutrition reviews 2014;72 Suppl 1():65-71
http://dx.doi.org/10.1111/nure.12150 https://pubmed.ncbi.nlm.nih.gov/25293545[56] Mathers M, Toumbourou JW, Catalano RF, Williams J, Patton GC. Consequences of youth tobacco use: a review of prospective behavioural studies. Addiction (Abingdon, England) 2006;101(7):948-58
https://pubmed.ncbi.nlm.nih.gov/16771887[57] Patten CA, Choi WS, Gillin JC, Pierce JP. Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics 2000;106(2):E23
https://pubmed.ncbi.nlm.nih.gov/10920179[58] Pasch KE, Latimer LA, Cance JD, Moe SG, Lytle LA. Longitudinal bi-directional relationships between sleep and youth substance use. Journal of youth and adolescence 2012;41(9):1184-96
http://dx.doi.org/10.1007/s10964-012-9784-5 https://pubmed.ncbi.nlm.nih.gov/22752878[59] O'Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behavioral sleep medicine 2005;3(3):113-33
https://pubmed.ncbi.nlm.nih.gov/15984914[60] Treyster Z, Gitterman B. Second hand smoke exposure in children: environmental factors, physiological effects, and interventions within pediatrics. Reviews on environmental health 2011;26(3):187-95
https://pubmed.ncbi.nlm.nih.gov/22206195[61] Wong MM, Robertson GC, Dyson RB. Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcoholism, clinical and experimental research 2015;39(2):355-62
http://dx.doi.org/10.1111/acer.12618 https://pubmed.ncbi.nlm.nih.gov/25598438[62] Roberts RE, Roberts CR, Duong HT. Sleepless in adolescence: prospective data on sleep deprivation, health and functioning. Journal of adolescence 2009;32(5):1045-57
http://dx.doi.org/10.1016/j.adolescence.2009.03.007 https://pubmed.ncbi.nlm.nih.gov/19361854[63] Wahlstrom K, Dretzke B, Gordon M, Peterson K, Edwards K, Gdula J. Examining the Impact of Later School Start Times on the Health and Academic Performance of High School Students: A Multi-Site Study Center for Applied Research and Educational Improvement. St Paul, MN: University of Minnesota. 2014
[64] Danner F, Phillips B. Adolescent sleep, school start times, and teen motor vehicle crashes. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2008;4(6):533-5
https://pubmed.ncbi.nlm.nih.gov/19110880[65] Labree LJWW, van de Mheen HD, Rutten FFHF, Rodenburg GG, Koopmans GTG, Foets MM. Sleep duration differences between children of migrant and native origins. Zeitschrift fur Gesundheitswissenschaften = Journal of public health 2015;23(3):149-156
https://pubmed.ncbi.nlm.nih.gov/26000233[66] Knutson KL. Sociodemographic and cultural determinants of sleep deficiency: implications for cardiometabolic disease risk. Social science & medicine (1982) 2013;79():7-15
http://dx.doi.org/10.1016/j.socscimed.2012.05.002 https://pubmed.ncbi.nlm.nih.gov/22682665[67] Mindell JA, Sadeh A, Kohyama J, How TH. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep medicine 2010;11(4):393-9
http://dx.doi.org/10.1016/j.sleep.2009.11.011 https://pubmed.ncbi.nlm.nih.gov/20223706[68] Olds T, Blunden S, Petkov J, Forchino F. The relationships between sex, age, geography and time in bed in adolescents: a meta-analysis of data from 23 countries. Sleep medicine reviews 2010;14(6):371-8
http://dx.doi.org/10.1016/j.smrv.2009.12.002 https://pubmed.ncbi.nlm.nih.gov/20207558[69] Schredl M, Reinhard I. Gender differences in nightmare frequency: a meta-analysis. Sleep medicine reviews 2011;15(2):115-21
http://dx.doi.org/10.1016/j.smrv.2010.06.002 https://pubmed.ncbi.nlm.nih.gov/20817509[70] Meijer AM, Habekothé HT, Van Den Wittenboer GL. Time in bed, quality of sleep and school functioning of children. Journal of sleep research 2000;9(2):145-53
https://pubmed.ncbi.nlm.nih.gov/10849241[71] Konofal E, Lecendreux M, Cortese S. Sleep and ADHD. Sleep medicine 2010;11(7):652-8
http://dx.doi.org/10.1016/j.sleep.2010.02.012 https://pubmed.ncbi.nlm.nih.gov/20620109[72] Sadeh A, Pergamin L, Bar-Haim Y. Sleep in children with attention-deficit hyperactivity disorder: a meta-analysis of polysomnographic studies. Sleep medicine reviews 2006;10(6):381-98
https://pubmed.ncbi.nlm.nih.gov/16846743[73] Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. Journal of the American Academy of Child and Adolescent Psychiatry 2009;48(9):894-908
http://dx.doi.org/10.1097/CHI.0b013e3181ac09c9 https://pubmed.ncbi.nlm.nih.gov/19625983[74] Bullock GL, Schall U. Dyssomnia in children diagnosed with attention deficit hyperactivity disorder: a critical review. The Australian and New Zealand journal of psychiatry 2005;39(5):373-7
https://pubmed.ncbi.nlm.nih.gov/15860025[75] Ivanenko A, Johnson K. Sleep disturbances in children with psychiatric disorders. Seminars in pediatric neurology 2008;15(2):70-8
http://dx.doi.org/10.1016/j.spen.2008.03.008 https://pubmed.ncbi.nlm.nih.gov/18555193[76] Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep medicine reviews 2012;16(3):231-41
http://dx.doi.org/10.1016/j.smrv.2011.05.005 https://pubmed.ncbi.nlm.nih.gov/21784678[77] Liu J, Zhang A, Li L. Sleep duration and overweight/obesity in children: review and implications for pediatric nursing. Journal for specialists in pediatric nursing : JSPN 2012;17(3):193-204
http://dx.doi.org/10.1111/j.1744-6155.2012.00332.x https://pubmed.ncbi.nlm.nih.gov/22734873[78] Kuhl ES, Clifford LM, Stark LJ. Obesity in preschoolers: behavioral correlates and directions for treatment. Obesity (Silver Spring, Md.) 2012;20(1):3-29
http://dx.doi.org/10.1038/oby.2011.201 https://pubmed.ncbi.nlm.nih.gov/21760634[79] Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring, Md.) 2008;16(2):265-74
http://dx.doi.org/10.1038/oby.2007.63 https://pubmed.ncbi.nlm.nih.gov/18239632[80] Cappuccio FP, Taggart FM, Kandala N-B, Currie A, Peile ED, Stranges S, Miller MA. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008;31(5):619-26
https://pubmed.ncbi.nlm.nih.gov/18517032[81] Hollway JA, Aman MG. Sleep correlates of pervasive developmental disorders: a review of the literature. Research in developmental disabilities 2011;32(5):1399-421
http://dx.doi.org/10.1016/j.ridd.2011.04.001 https://pubmed.ncbi.nlm.nih.gov/21570809[82] Valrie CR, Bromberg MH, Palermo T, Schanberg LE. A systematic review of sleep in pediatric pain populations. Journal of developmental and behavioral pediatrics : JDBP 2013;34(2):120-8
http://dx.doi.org/10.1097/DBP.0b013e31827d5848 https://pubmed.ncbi.nlm.nih.gov/23369958[83] Tietze A-L, Blankenburg M, Hechler T, Michel E, Koh M, Schlüter B, Zernikow B. Sleep disturbances in children with multiple disabilities. Sleep medicine reviews 2012;16(2):117-27
http://dx.doi.org/10.1016/j.smrv.2011.03.006 https://pubmed.ncbi.nlm.nih.gov/21620745[84] Yilmaz E, Sedky K, Bennett DS. The relationship between depressive symptoms and obstructive sleep apnea in pediatric populations: a meta-analysis. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2013;9(11):1213-20
http://dx.doi.org/10.5664/jcsm.3178 https://pubmed.ncbi.nlm.nih.gov/24235907[85] Kowatch RA, Youngstrom EA, Danielyan A, Findling RL. Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar disorders 2005;7(6):483-96
https://pubmed.ncbi.nlm.nih.gov/16403174[86] Cairns KE, Yap MBH, Pilkington PD, Jorm AF. Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. Journal of affective disorders 2014;169():61-75
http://dx.doi.org/10.1016/j.jad.2014.08.006 https://pubmed.ncbi.nlm.nih.gov/25154536[87] Augustinavicius JLS, Zanjani A, Zakzanis KK, Shapiro CM. Polysomnographic features of early-onset depression: a meta-analysis. Journal of affective disorders 2014;158():11-8
http://dx.doi.org/10.1016/j.jad.2013.12.009 https://pubmed.ncbi.nlm.nih.gov/24655760[88] Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. The Journal of clinical psychiatry 2012;73(9):e1160-7
http://dx.doi.org/10.4088/JCP.11r07586 https://pubmed.ncbi.nlm.nih.gov/23059158[89] Churchill SS, Kieckhefer GM, Bjornson KF, Herting JR. Relationship between sleep disturbance and functional outcomes in daily life habits of children with Down syndrome. Sleep 2015;38(1):61-71
http://dx.doi.org/10.5665/sleep.4326 https://pubmed.ncbi.nlm.nih.gov/25325444[90] van Golde EGA, Gutter T, de Weerd AW. Sleep disturbances in people with epilepsy; prevalence, impact and treatment. Sleep medicine reviews 2011;15(6):357-68
http://dx.doi.org/10.1016/j.smrv.2011.01.002 https://pubmed.ncbi.nlm.nih.gov/21439869[91] Charuvastra A, Cloitre M. Safe enough to sleep: sleep disruptions associated with trauma, posttraumatic stress, and anxiety in children and adolescents. Child and adolescent psychiatric clinics of North America 2009;18(4):877-91
http://dx.doi.org/10.1016/j.chc.2009.04.002 https://pubmed.ncbi.nlm.nih.gov/19836694[92] Camfferman D, Kennedy JD, Gold M, Martin AJ, Winwood P, Lushington K. Eczema, sleep, and behavior in children. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2010;6(6):581-8
https://pubmed.ncbi.nlm.nih.gov/21206547[93] Camfferman D, Kennedy JD, Gold M, Simpson C, Lushington K. Sleep and neurocognitive functioning in children with eczema. International journal of psychophysiology : official journal of the International Organization of Psychophysiology 2013;89(2):265-72
http://dx.doi.org/10.1016/j.ijpsycho.2013.01.006 https://pubmed.ncbi.nlm.nih.gov/23353660[94] Ryborg CT, Søndergaard J, Lous J, Munck A, Larsen PV, Thomsen JL. Associations between symptoms, clinical findings and the short-term prognosis among children with otitis media: a cohort study. International journal of pediatric otorhinolaryngology 2013;77(2):210-5
http://dx.doi.org/10.1016/j.ijporl.2012.10.023 https://pubmed.ncbi.nlm.nih.gov/23200872[95] McCormick DP, Jennings K, Ede LC, Alvarez-Fernandez P, Patel J, Chonmaitree T. Use of symptoms and risk factors to predict acute otitis media in infants. International journal of pediatric otorhinolaryngology 2016;81():55-9
http://dx.doi.org/10.1016/j.ijporl.2015.12.002 https://pubmed.ncbi.nlm.nih.gov/26810291[96] Laine MK, Tähtinen PA, Ruuskanen O, Huovinen P, Ruohola A. Symptoms or symptom-based scores cannot predict acute otitis media at otitis-prone age. Pediatrics 2010;125(5):e1154-61
http://dx.doi.org/10.1542/peds.2009-2689 https://pubmed.ncbi.nlm.nih.gov/20368317[97] Üçer O, Gümüş B. Quantifying subjective assessment of sleep quality, quality of life and depressed mood in children with enuresis. World journal of urology 2014;32(1):239-43
http://dx.doi.org/10.1007/s00345-013-1193-1 https://pubmed.ncbi.nlm.nih.gov/24150187[98] Azevedo Soster L, Alves R, Fagundes SN, Koch VHK, Bruni O. Sleep disturbances associated with sleep enuresis: A questionnaire study. European journal of paediatric neurology : EJPN : official journal of the European Paediatric Neurology Society 2016;20(2):282-285
http://dx.doi.org/10.1016/j.ejpn.2015.11.014 https://pubmed.ncbi.nlm.nih.gov/26732069[99] Costigan SA, Barnett L, Plotnikoff RC, Lubans DR. The health indicators associated with screen-based sedentary behavior among adolescent girls: a systematic review. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 2013;52(4):382-92
http://dx.doi.org/10.1016/j.jadohealth.2012.07.018 https://pubmed.ncbi.nlm.nih.gov/23299000[100] Owens J, , . Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics 2014;134(3):e921-32
http://dx.doi.org/10.1542/peds.2014-1696 https://pubmed.ncbi.nlm.nih.gov/25157012[101] Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep medicine reviews 2015;21():50-8
http://dx.doi.org/10.1016/j.smrv.2014.07.007 https://pubmed.ncbi.nlm.nih.gov/25193149[102] Kirby MF, Maggi S, D'Angiulli A. School Start Times and the Sleep–Wake Cycle of Adolescents Educational Researcher 2011;40(2):56
https://www.researchgate.net/publication/258134857_School_Start_Times_and_the_Sleep-Wake_Cycle_of_Adolescents[103] Kelley P, Lockley SW, Foster RG, Kelley J. Synchronizing education to adolescent biology: 'Let teens sleep, start school later' Learning Media and Technology 2014;40(2):1
https://www.researchgate.net/publication/271991912_Synchronizing_education_to_adolescent_biology_'let_teens_sleep_start_school_later'[104] Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children. Sleep 2005;28(12):1568-77
https://pubmed.ncbi.nlm.nih.gov/16408417[105] Cornelius LJ. Health habits of school-age children. Journal of health care for the poor and underserved 1991;2(3):374-95
https://pubmed.ncbi.nlm.nih.gov/1772949[106] McLaughlin Crabtree V, Beal Korhonen J, Montgomery-Downs HE, Faye Jones V, O'Brien LM, Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep medicine 2005;6(4):319-24
https://pubmed.ncbi.nlm.nih.gov/15978515[107] Marco CA, Wolfson AR, Sparling M, Azuaje A. Family socioeconomic status and sleep patterns of young adolescents. Behavioral sleep medicine 2011;10(1):70-80
http://dx.doi.org/10.1080/15402002.2012.636298 https://pubmed.ncbi.nlm.nih.gov/22250780[108] Guérin N, Reinberg A, Testu F, Boulenguiez S, Mechkouri M, Touitou Y. Role of school schedule, age, and parental socioeconomic status on sleep duration and sleepiness of Parisian children. Chronobiology international 2001;18(6):1005-17
https://pubmed.ncbi.nlm.nih.gov/11777075[109] Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep medicine reviews 2008;12(4):289-98
http://dx.doi.org/10.1016/j.smrv.2008.03.001 https://pubmed.ncbi.nlm.nih.gov/18485764[110] Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring, Md.) 2008;16(3):643-53
http://dx.doi.org/10.1038/oby.2007.118 https://pubmed.ncbi.nlm.nih.gov/18239586[111] L'Hoir MP, Vlasblom E, Boere-Boonekamp MM, van Dommelen P, Schmelt D, Dreiskaemper D, Naul R. Slaap en overgewicht in Europees onderzoek: Gezonde Kinderen in een Gezonde Kindomgeving (GKGK). Tijdschrift Jeugdgezondheidszorg 2012;44(6):102
[112] Douglas PS, Hill PS. Behavioral sleep interventions in the first six months of life do not improve outcomes for mothers or infants: a systematic review. Journal of developmental and behavioral pediatrics : JDBP 2013;34(7):497-507
http://dx.doi.org/10.1097/DBP.0b013e31829cafa6 https://pubmed.ncbi.nlm.nih.gov/24042081[113] Blunden SL, Chapman J, Rigney GA. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep medicine reviews 2012;16(4):355-70
http://dx.doi.org/10.1016/j.smrv.2011.08.002 https://pubmed.ncbi.nlm.nih.gov/22104441[114] Bryanton J, Beck CT, Montelpare W. Postnatal parental education for optimizing infant general health and parent-infant relationships. The Cochrane database of systematic reviews 2013
http://dx.doi.org/10.1002/14651858.CD004068.pub4 https://pubmed.ncbi.nlm.nih.gov/24284872[115] Bakker-Camu GJW, Nawijn L, van Sleuwen BE, L'Hoir MP. Preventie van slaapproblemen bij jonge kinderen. Review van de effectieve elementen. Tijdschrift Jeugdgezondheidszorg 2011;43(2):26
[116] Crichton GE, Symon B. Behavioral Management of Sleep Problems in Infants Under 6 Months--What Works? Journal of developmental and behavioral pediatrics : JDBP 2016;37(2):164-71
http://dx.doi.org/10.1097/DBP.0000000000000257 https://pubmed.ncbi.nlm.nih.gov/26836644[117] Allen SL, Howlett MD, Coulombe JA, Corkum PV. ABCs of SLEEPING: A review of the evidence behind pediatric sleep practice recommendations. Sleep medicine reviews 2016;29():1-14
http://dx.doi.org/10.1016/j.smrv.2015.08.006 https://pubmed.ncbi.nlm.nih.gov/26551999[118] Bennett C, Underdown A, Barlow J. Massage for promoting mental and physical health in typically developing infants under the age of six months. The Cochrane database of systematic reviews 2013;2013(4):CD005038
http://dx.doi.org/10.1002/14651858.CD005038.pub3 https://pubmed.ncbi.nlm.nih.gov/23633323[119] Underdown A, Barlow J, Stewart-Brown S. Tactile stimulation in physically healthy infants: Results of a systematic review. Journal of Reproductive and Infant Psychology 2010;28(1):11
[120] van der Lely S, Frey S, Garbazza C, Wirz-Justice A, Jenni OG, Steiner R, Wolf S, Cajochen C, Bromundt V, Schmidt C. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 2015;56(1):113-9
http://dx.doi.org/10.1016/j.jadohealth.2014.08.002 https://pubmed.ncbi.nlm.nih.gov/25287985[121] Burkhart K, Phelps JR. Amber lenses to block blue light and improve sleep: a randomized trial. Chronobiology international 2009;26(8):1602-12
http://dx.doi.org/10.3109/07420520903523719 https://pubmed.ncbi.nlm.nih.gov/20030543[122] Chellappa SL, Gordijn MCM, Cajochen C. Can light make us bright? Effects of light on cognition and sleep. Progress in brain research 2011;190():119-33
http://dx.doi.org/10.1016/B978-0-444-53817-8.00007-4 https://pubmed.ncbi.nlm.nih.gov/21531248[123] Spencer JA, Moran DJ, Lee A, Talbert D. White noise and sleep induction. Archives of disease in childhood 1990;65(1):135-7
https://pubmed.ncbi.nlm.nih.gov/2405784[124] Forquer LM, Johnson C. Continuous White Noise to Reduce Resistance Going to Sleep and Night Wakings in Toddlers Child & Family Behavior Therapy 2005;27(2):1
[125] Waumans RC, Terwee CB, Van den Berg G, Knol DL, Van Litsenburg RRL, Gemke RJBJ. Sleep and sleep disturbance in children: Reliability and validity of the Dutch version of the Child Sleep Habits Questionnaire. Sleep 2010;33(6):841-5
https://pubmed.ncbi.nlm.nih.gov/20550026[126] Dewald JF, Short MA, Gradisar M, Oort FJ, Meijer AM. The Chronic Sleep Reduction Questionnaire (CSRQ): a cross-cultural comparison and validation in Dutch and Australian adolescents. Journal of sleep research 2012;21(5):584-94
http://dx.doi.org/10.1111/j.1365-2869.2012.00999.x https://pubmed.ncbi.nlm.nih.gov/22329363[127] Ramdurg S. Kleine-Levin syndrome: Etiology, diagnosis, and treatment. Annals of Indian Academy of Neurology 2010;13(4):241-6
http://dx.doi.org/10.4103/0972-2327.74185 https://pubmed.ncbi.nlm.nih.gov/21264130[128] Simakajornboon N, Kheirandish-Gozal L, Gozal D. Diagnosis and management of restless legs syndrome in children. Sleep medicine reviews 2009;13(2):149-56
http://dx.doi.org/10.1016/j.smrv.2008.12.002 https://pubmed.ncbi.nlm.nih.gov/19186083[129] Meijer AM, Hofman W. Assessment en protocollaire behandeling van slaapproblemen bij kinderen Protocollaire behandelingen voor kinderen met psychische klachten 2014
[130] Morgenthaler TI, Owens J, Alessi C, Boehlecke B, Brown TM, Coleman J, Friedman L, Kapur VK, Lee-Chiong T, Pancer J, Swick TJ, . Practice parameters for behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep 2006;29(10):1277-81
https://pubmed.ncbi.nlm.nih.gov/17068980[131] Brown CA, Kuo M, Phillips L, Berry R, Tan M. Non-pharmacological sleep interventions for youth with chronic health conditions: a critical review of the methodological quality of the evidence. Disability and rehabilitation 2013;35(15):1221-55
http://dx.doi.org/10.3109/09638288.2012.723788 https://pubmed.ncbi.nlm.nih.gov/23050860[132] Escalona A, Field T, Singer-Strunck R, Cullen C, Hartshorn K. Brief report: improvements in the behavior of children with autism following massage therapy. Journal of autism and developmental disorders 2001;31(5):513-6
https://pubmed.ncbi.nlm.nih.gov/11794416[133] Dobson D, Lucassen PLBJ, Miller JJ, Vlieger AM, Prescott P, Lewith G. Manipulative therapies for infantile colic. The Cochrane database of systematic reviews 2012;12():CD004796
http://dx.doi.org/10.1002/14651858.CD004796.pub2 https://pubmed.ncbi.nlm.nih.gov/23235617[134] McRury JM, Zolotor AJ. A randomized, controlled trial of a behavioral intervention to reduce crying among infants. Journal of the American Board of Family Medicine : JABFM 2010;23(3):315-22
http://dx.doi.org/10.3122/jabfm.2010.03.090142 https://pubmed.ncbi.nlm.nih.gov/20453177[135] Quach J, Hiscock H, Ukoumunne OC, Wake M. A brief sleep intervention improves outcomes in the school entry year: a randomized controlled trial. Pediatrics 2011;128(4):692-701
http://dx.doi.org/10.1542/peds.2011-0409 https://pubmed.ncbi.nlm.nih.gov/21890825[136] Sciberras E, Fulton M, Efron D, Oberklaid F, Hiscock H. Managing sleep problems in school aged children with ADHD: a pilot randomised controlled trial. Sleep medicine 2011;12(9):932-5
http://dx.doi.org/10.1016/j.sleep.2011.02.006 https://pubmed.ncbi.nlm.nih.gov/22005602[137] Moore BA, Friman PC, Fruzzetti AE, MacAleese K. Brief report: evaluating the Bedtime Pass Program for child resistance to bedtime--a randomized, controlled trial. Journal of pediatric psychology 2007;32(3):283-7
https://pubmed.ncbi.nlm.nih.gov/16899650[138] Gradisar M, Dohnt H, Gardner G, Paine S, Starkey K, Menne A, Slater A, Wright H, Hudson JL, Weaver E, Trenowden S. A randomized controlled trial of cognitive-behavior therapy plus bright light therapy for adolescent delayed sleep phase disorder. Sleep 2011;34(12):1671-80
http://dx.doi.org/10.5665/sleep.1432 https://pubmed.ncbi.nlm.nih.gov/22131604[139] de Bruin EJ, Bögels SM, Oort FJ, Meijer AM. Efficacy of Cognitive Behavioral Therapy for Insomnia in Adolescents: A Randomized Controlled Trial with Internet Therapy, Group Therapy and A Waiting List Condition. Sleep 2015;38(12):1913-26
http://dx.doi.org/10.5665/sleep.5240 https://pubmed.ncbi.nlm.nih.gov/26158889[140] de Bruin EJ, Oort FJ, Bögels SM, Meijer AM. Efficacy of internet and group-administered cognitive behavioral therapy for insomnia in adolescents: a pilot study. Behavioral sleep medicine 2014;12(3):235-54
http://dx.doi.org/10.1080/15402002.2013.784703 https://pubmed.ncbi.nlm.nih.gov/23767888[141] Bendz LM, Scates AC. Melatonin treatment for insomnia in pediatric patients with attention-deficit/hyperactivity disorder. The Annals of pharmacotherapy 2010;44(1):185-91
http://dx.doi.org/10.1345/aph.1M365 https://pubmed.ncbi.nlm.nih.gov/20028959[142] van Geijlswijk IM, Korzilius HPLM, Smits MG. The use of exogenous melatonin in delayed sleep phase disorder: a meta-analysis. Sleep 2010;33(12):1605-14
https://pubmed.ncbi.nlm.nih.gov/21120122[143] Barrett JR, Tracy DK, Giaroli G. To sleep or not to sleep: a systematic review of the literature of pharmacological treatments of insomnia in children and adolescents with attention-deficit/hyperactivity disorder. Journal of child and adolescent psychopharmacology 2013;23(10):640-7
http://dx.doi.org/10.1089/cap.2013.0059 https://pubmed.ncbi.nlm.nih.gov/24261659[144] Van der Heijden KB, Smits MG, Van Someren EJW, Ridderinkhof KR, Gunning WB. Effect of melatonin on sleep, behavior, and cognition in ADHD and chronic sleep-onset insomnia. Journal of the American Academy of Child and Adolescent Psychiatry 2007;46(2):233-41
https://pubmed.ncbi.nlm.nih.gov/17242627[145] Khan S, Heussler H, McGuire T, Dakin C, Pache D, Cooper D, Norris R, Flenady V, Charles B. Melatonin for non-respiratory sleep disorders in visually impaired children. The Cochrane database of systematic reviews 2011
http://dx.doi.org/10.1002/14651858.CD008473.pub2 https://pubmed.ncbi.nlm.nih.gov/22071850[146] Hoebert M, van der Heijden KB, van Geijlswijk IM, Smits MG. Long-term follow-up of melatonin treatment in children with ADHD and chronic sleep onset insomnia. Journal of pineal research 2009;47(1):1-7
http://dx.doi.org/10.1111/j.1600-079X.2009.00681.x https://pubmed.ncbi.nlm.nih.gov/19486273[147] Braam W, Smits MG, Didden R, Korzilius H, Van Geijlswijk IM, Curfs LMG. Exogenous melatonin for sleep problems in individuals with intellectual disability: a meta-analysis. Developmental medicine and child neurology 2009;51(5):340-9
http://dx.doi.org/10.1111/j.1469-8749.2008.03244.x https://pubmed.ncbi.nlm.nih.gov/19379289[148] Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, Vohra S, Klassen TP, Baker G. Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. BMJ (Clinical research ed.) 2006;332(7538):385-93
https://pubmed.ncbi.nlm.nih.gov/16473858[149] Guénolé F, Godbout R, Nicolas A, Franco P, Claustrat B, Baleyte J-M. Melatonin for disordered sleep in individuals with autism spectrum disorders: systematic review and discussion. Sleep medicine reviews 2011;15(6):379-87
http://dx.doi.org/10.1016/j.smrv.2011.02.001 https://pubmed.ncbi.nlm.nih.gov/21393033[150] Rossignol DA, Frye RE. Melatonin in autism spectrum disorders: a systematic review and meta-analysis. Developmental medicine and child neurology 2011;53(9):783-792
http://dx.doi.org/10.1111/j.1469-8749.2011.03980.x https://pubmed.ncbi.nlm.nih.gov/21518346[151] Malow BA, Byars K, Johnson K, Weiss S, Bernal P, Goldman SE, Panzer R, Coury DL, Glaze DG, . A practice pathway for the identification, evaluation, and management of insomnia in children and adolescents with autism spectrum disorders. Pediatrics 2012;130 Suppl 2(Suppl 2):S106-24
http://dx.doi.org/10.1542/peds.2012-0900I https://pubmed.ncbi.nlm.nih.gov/23118242[152] Fernández-San-Martín MI, Masa-Font R, Palacios-Soler L, Sancho-Gómez P, Calbó-Caldentey C, Flores-Mateo G. Effectiveness of Valerian on insomnia: a meta-analysis of randomized placebo-controlled trials. Sleep medicine 2010;11(6):505-11
http://dx.doi.org/10.1016/j.sleep.2009.12.009 https://pubmed.ncbi.nlm.nih.gov/20347389[153] van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, Kuis W, Schulpen TWJ, L'Hoir MP. Swaddling: a systematic review. Pediatrics 2007;120(4):e1097-106
https://pubmed.ncbi.nlm.nih.gov/17908730[154] Bootzin RR, Stevens SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clinical psychology review 2005;25(5):629-44
https://pubmed.ncbi.nlm.nih.gov/15953666[155] Britton WB, Bootzin RR, Cousins JC, Hasler BP, Peck T, Shapiro SL. The contribution of mindfulness practice to a multicomponent behavioral sleep intervention following substance abuse treatment in adolescents: a treatment-development study. Substance abuse 2010;31(2):86-97
http://dx.doi.org/10.1080/08897071003641297 https://pubmed.ncbi.nlm.nih.gov/20408060[156] Bei B, Byrne ML, Ivens C, Waloszek J, Woods MJ, Dudgeon P, Murray G, Nicholas CL, Trinder J, Allen NB. Pilot study of a mindfulness-based, multi-component, in-school group sleep intervention in adolescent girls. Early intervention in psychiatry 2013;7(2):213-20
http://dx.doi.org/10.1111/j.1751-7893.2012.00382.x https://pubmed.ncbi.nlm.nih.gov/22759744[157] Schregardus R. Kinderen met slaapproblemen. Amsterdam: Uitgeverij Boom
[158] Sadeh A, Mindell JA, Owens J. Why care about sleep of infants and their parents? Sleep medicine reviews 2011;15(5):335-7
http://dx.doi.org/10.1016/j.smrv.2011.03.001 https://pubmed.ncbi.nlm.nih.gov/21612956[159] Middlemiss W, Granger DA, Goldberg WA. Response to "let's help parents help themselves: a letter to the editor supporting the safety of behavioural sleep techniques". Early human development 2013;89(1):41-2
http://dx.doi.org/10.1016/j.earlhumdev.2012.07.016 https://pubmed.ncbi.nlm.nih.gov/22889752[160] Price A, Hiscock H, Gradisar M. Let's help parents help themselves: a letter to the editor supporting the safety of behavioural sleep techniques. Early human development 2013;89(1):39-40
http://dx.doi.org/10.1016/j.earlhumdev.2012.07.018 https://pubmed.ncbi.nlm.nih.gov/22883341[161] Middlemiss W, Granger DA, Goldberg WA, Nathans L. Asynchrony of mother-infant hypothalamic-pituitary-adrenal axis activity following extinction of infant crying responses induced during the transition to sleep. Early human development 2012;88(4):227-32
http://dx.doi.org/10.1016/j.earlhumdev.2011.08.010 https://pubmed.ncbi.nlm.nih.gov/21945361[162] Price AMH, Wake M, Ukoumunne OC, Hiscock H. Five-year follow-up of harms and benefits of behavioral infant sleep intervention: randomized trial. Pediatrics 2012;130(4):643-51
http://dx.doi.org/10.1542/peds.2011-3467 https://pubmed.ncbi.nlm.nih.gov/22966034[163] Boer F. Slaapproblemen bij kinderen: Kinderpsychologie in de praktijk. Lannoo-Meulenhoff Belgium 2013
[164] Karp HN. Re: a randomized, controlled trial of a behavioral intervention to reduce crying among infants. Journal of the American Board of Family Medicine : JABFM 2010;23(5):689-90; author reply 690-1
http://dx.doi.org/10.3122/jabfm.2010.05.100139 https://pubmed.ncbi.nlm.nih.gov/20823369[165] Harrington JW, Logan S, Harwell C, Gardner J, Swingle J, McGuire E, Santos R. Effective analgesia using physical interventions for infant immunizations. Pediatrics 2012;129(5):815-22
http://dx.doi.org/10.1542/peds.2011-1607 https://pubmed.ncbi.nlm.nih.gov/22508924[166] de Bruin E, Waterman D, Meijer AM. SlimSlapen: Cognitieve gedragstherapie voor insomnia (CGT-i) bij adolescenten. In: Braet C, Bögels S, eds. Protocollaire behandelingen voor kinderen en adolescenten met psychische klachten. 1st ed. Amsterdam: Boom 2013
[167] Vlasblom E, Beltman M. Rapportage Praktijktest richtlijn Gezonde slaap en slaapproblemen bij kinderen. 2016
http://dx.doi.org/TNO,%20Leiden[168] Krom M. De relatie tussen de slaapduur en het werkgeheugen van kinderen van 8-9 jaar en kinderen van 10-11 jaar oud. 2012
http://dx.doi.org/Universiteit%20Leiden[169] LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics 2005;115(1 Suppl):257-65
https://pubmed.ncbi.nlm.nih.gov/15866860[170] Meijer AM. Chronic sleep reduction, functioning at school and school achievement in preadolescents. Journal of sleep research 2008;17(4):395-405
http://dx.doi.org/10.1111/j.1365-2869.2008.00677.x https://pubmed.ncbi.nlm.nih.gov/19021856[171] Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension on sleep and cognitive performance in adolescents with chronic sleep reduction: an experimental study. Sleep medicine 2013;14(6):510-7
http://dx.doi.org/10.1016/j.sleep.2013.01.012 https://pubmed.ncbi.nlm.nih.gov/23523432[172] Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension and sleep hygiene advice on sleep and depressive symptoms in adolescents: a randomized controlled trial. Journal of child psychology and psychiatry, and allied disciplines 2014;55(3):273-83
http://dx.doi.org/10.1111/jcpp.12157 https://pubmed.ncbi.nlm.nih.gov/24252173[173] Dewald-Kaufmann JF, Oort FJ, Bögels SM, Meijer AM. Why sleep matters: Differences in daytime functioning between adolescents with low and high chronic sleep reduction and short and long sleep durations. Journal of Cognitive and Behavioral Psychotherapies 2013;13(1a):171
[174] Hunziker UA, Barr RG. Increased carrying reduces infant crying: a randomized controlled trial. Pediatrics 1986;77(5):641-8
https://pubmed.ncbi.nlm.nih.gov/3517799[175] Müller S, Hemmi MH, Wilhelm FH, Barr RG, Schneider S. Parental report of infant sleep behavior by electronic versus paper-and-pencil diaries, and their relationship to actigraphic sleep measurement. Journal of sleep research 2011;20(4):598-605
http://dx.doi.org/10.1111/j.1365-2869.2011.00926.x https://pubmed.ncbi.nlm.nih.gov/21707809[176] Werner H, Molinari L, Guyer C, Jenni OG. Agreement rates between actigraphy, diary, and questionnaire for children's sleep patterns. Archives of pediatrics & adolescent medicine 2008;162(4):350-8
http://dx.doi.org/10.1001/archpedi.162.4.350 https://pubmed.ncbi.nlm.nih.gov/18391144[177] Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, Morin CM. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep 2012;35(2):287-302
http://dx.doi.org/10.5665/sleep.1642 https://pubmed.ncbi.nlm.nih.gov/22294820[178] Erickson JM. Approaches to measure sleep-wake disturbances in adolescents with cancer. Journal of pediatric nursing 2009;24(4):255-69
http://dx.doi.org/10.1016/j.pedn.2008.03.004 https://pubmed.ncbi.nlm.nih.gov/19632503[179] Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, Martin JL. Evidence for the validity of a sleep habits survey for adolescents. Sleep 2003;26(2):213-6
https://pubmed.ncbi.nlm.nih.gov/12683482[180] Bruni O, Alonso-Alconada D, Besag F, Biran V, Braam W, Cortese S, Moavero R, Parisi P, Smits M, Van der Heijden K, Curatolo P. Current role of melatonin in pediatric neurology: clinical recommendations. European journal of paediatric neurology : EJPN : official journal of the European Paediatric Neurology Society 2015;19(2):122-33
http://dx.doi.org/10.1016/j.ejpn.2014.12.007 https://pubmed.ncbi.nlm.nih.gov/25553845[181] Cohen D, Bonnot O, Bodeau N, Consoli A, Laurent C. Adverse effects of second-generation antipsychotics in children and adolescents: a Bayesian meta-analysis. Journal of clinical psychopharmacology 2012;32(3):309-16
http://dx.doi.org/10.1097/JCP.0b013e3182549259 https://pubmed.ncbi.nlm.nih.gov/22544019[182] Owens JA, Moturi S. Pharmacologic treatment of pediatric insomnia. Child and adolescent psychiatric clinics of North America 2009;18(4):1001-16
http://dx.doi.org/10.1016/j.chc.2009.04.009 https://pubmed.ncbi.nlm.nih.gov/19836701[183] Cheng JYW, Chen RYL, Ko JSN, Ng EML. Efficacy and safety of atomoxetine for attention-deficit/hyperactivity disorder in children and adolescents-meta-analysis and meta-regression analysis. Psychopharmacology 2007;194(2):197-209
https://pubmed.ncbi.nlm.nih.gov/17572882[184] Cortese S, Holtmann M, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Dittmann RW, Graham J, Taylor E, Sergeant J, . Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents. Journal of child psychology and psychiatry, and allied disciplines 2013;54(3):227-46
http://dx.doi.org/10.1111/jcpp.12036 https://pubmed.ncbi.nlm.nih.gov/23294014[185] Fietta P, Fietta P, Delsante G. Central nervous system effects of natural and synthetic glucocorticoids. Psychiatry and clinical neurosciences 2009;63(5):613-22
http://dx.doi.org/10.1111/j.1440-1819.2009.02005.x https://pubmed.ncbi.nlm.nih.gov/19788629[186] Owens JA, Babcock D, Blumer J, Chervin R, Ferber R, Goetting M, Glaze D, Ivanenko A, Mindell J, Rappley M, Rosen C, Sheldon S. The use of pharmacotherapy in the treatment of pediatric insomnia in primary care: rational approaches. A consensus meeting summary. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2005;1(1):49-59
https://pubmed.ncbi.nlm.nih.gov/17561616[187] Kempler L, Sharpe L, Miller CB, Bartlett DJ. Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? A systematic review and meta-analysis of randomised controlled trials. Sleep medicine reviews 2016;29():15-22
http://dx.doi.org/10.1016/j.smrv.2015.08.002 https://pubmed.ncbi.nlm.nih.gov/26555938[188] Douglas PS. High level evidence does not support first wave behavioural approaches to parent-infant sleep Sleep Medicine Reviews 2015;29():
[189] Douglas P, Whittingham K. Response to 'sleeping like a baby? infant sleep: Impact on care givers and current controversies'. Journal of paediatrics and child health 2015;51(2):234
http://dx.doi.org/10.1111/jpc.12835 https://pubmed.ncbi.nlm.nih.gov/25677489[190] Gradisar M, Jackson K, Spurrier NJ, Gibson J, Whitham J, Williams AS, Dolby R, Kennaway DJ. Behavioral Interventions for Infant Sleep Problems: A Randomized Controlled Trial. Pediatrics 2016;137(6):
http://dx.doi.org/10.1542/peds.2015-1486 https://pubmed.ncbi.nlm.nih.gov/27221288[191] Hiscock H, Fisher J. Sleeping like a baby? Infant sleep: impact on caregivers and current controversies. Journal of paediatrics and child health 2015;51(4):361-4
http://dx.doi.org/10.1111/jpc.12752 https://pubmed.ncbi.nlm.nih.gov/25293637[192] Middlemiss W, Yaure R, Huey EL. Translating research-based knowledge about infant sleep into practice. Journal of the American Association of Nurse Practitioners 2015;27(6):328-37
http://dx.doi.org/10.1002/2327-6924.12159 https://pubmed.ncbi.nlm.nih.gov/25088326[193] Narvaez D. The Ethics of Early Life Care: The Harms of Sleep Training Clinical Lactation 2013;4(2):66
[194] Crncec R, Matthey S, Nemeth D. Infant sleep problems and emotional health: A review of two behavioural approaches Journal of Reproductive and Infant Psychology 2010;28(1):44
[195] Blunden SL, Thompson KR, Dawson D. Behavioural sleep treatments and night time crying in infants: challenging the status quo. Sleep medicine reviews 2011;15(5):327-34
http://dx.doi.org/10.1016/j.smrv.2010.11.002 https://pubmed.ncbi.nlm.nih.gov/21295501[196] Barlow J, National Scientific Council on the Developing Child. Excessive stress disrupts the development of brain architecture. Journal of Children's Services 2014;9(2):143
[197] Ha T, Granger DA. Family Relations, Stress, and Vulnerability: Biobehavioral Implications for Prevention and Practice Family Relations 2016;65(1):9
[198] Jansen J, Beijers R, Riksen-Walraven M, de Weerth C. Cortisol reactivity in young infants. Psychoneuroendocrinology 2010;35(3):329-38
http://dx.doi.org/10.1016/j.psyneuen.2009.07.008 https://pubmed.ncbi.nlm.nih.gov/19651476[199] Beijers R, Jansen J, Riksen-Walraven M, de Weerth C. Attachment and infant night waking: a longitudinal study from birth through the first year of life. Journal of developmental and behavioral pediatrics : JDBP 2011;32(9):635-43
http://dx.doi.org/10.1097/DBP.0b013e318228888d https://pubmed.ncbi.nlm.nih.gov/21743349[200] Bélanger M-È, Bernier A, Simard V, Bordeleau S, Carrier J. Viii. Attachment and sleep among toddlers: disentangling attachment security and dependency. Monographs of the Society for Research in Child Development 2015;80(1):125-40
http://dx.doi.org/10.1111/mono.12148 https://pubmed.ncbi.nlm.nih.gov/25704739[201] Higley E, Dozier M. Nighttime maternal responsiveness and infant attachment at one year. Attachment & human development 2009;11(4):347-63
http://dx.doi.org/10.1080/14616730903016979 https://pubmed.ncbi.nlm.nih.gov/19603300[202] McNamara P, Belsky J, Fearon P. Infant sleep disorders and attachment: Sleep problems in infants with insecure-resistant versus insecure-avoidant attachments to mother. Sleep Hypnosis 2003;5(1):17
[203] Morrell J, Steele H. The role of attachment security, temperament, maternal perception, and care-giving behavior in persistent infant sleeping problems Infant mental health journal 2003;24(5):447
[204] Mileva-Seitz VR, Luijk MPCM, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Jaddoe VWV, Hofman A, Verhulst FC, Tiemeier H. ASSOCIATION BETWEEN INFANT NIGHTTIME-SLEEP LOCATION AND ATTACHMENT SECURITY: NO EASY VERDICT. Infant mental health journal 2016;37(1):5-16
http://dx.doi.org/10.1002/imhj.21547 https://pubmed.ncbi.nlm.nih.gov/26719041[205] Pennestri M-H, Moss E, O'Donnell K, Lecompte V, Bouvette-Turcot A-A, Atkinson L, Minde K, Gruber R, Fleming AS, Meaney MJ, Gaudreau H, . Establishment and consolidation of the sleep-wake cycle as a function of attachment pattern. Attachment & human development 2015;17(1):23-42
http://dx.doi.org/10.1080/14616734.2014.953963 https://pubmed.ncbi.nlm.nih.gov/25231054[206] Zentall SR, Braungart-Rieker JM, Ekas NV, Lickenbrock DM. Longitudinal assessment of sleep–wake regulation and attachment security with parents. Infant and Child Development 2012;21(5):443
[207] Simard V, Bernier A, Bélanger M-È, Carrier J. Infant attachment and toddlers' sleep assessed by maternal reports and actigraphy: different measurement methods yield different relations. Journal of pediatric psychology 2013;38(5):473-83
http://dx.doi.org/10.1093/jpepsy/jst001 https://pubmed.ncbi.nlm.nih.gov/23428653[208] Cronin A, Halligan SL, Murray L. Maternal psychosocial adversity and the longitudinal development of infant sleep. Infancy 2008;13(5):469
[209] Sheridan A, Murray L, Cooper PJ, Evangeli M, Byram V, Halligan SL. A longitudinal study of child sleep in high and low risk families: relationship to early maternal settling strategies and child psychological functioning. Sleep medicine 2013;14(3):266-73
http://dx.doi.org/10.1016/j.sleep.2012.11.006 https://pubmed.ncbi.nlm.nih.gov/23337072[210] Morrell J, Cortina-Borja M. The developmental change in strategies parents employ to settle young children to sleep, and their relationship to infant sleeping problems, as assessed by a new questionnaire: the Parental Interactive Bedtime Behaviour Scale Infant and Child Development 2002;11(1):17
[211] Cowie J, Palmer CA, Hussain H, Alfano CA. Parental Involvement in Infant Sleep Routines Predicts Differential Sleep Patterns in Children With and Without Anxiety Disorders. Child psychiatry and human development 2016;47(4):636-46
http://dx.doi.org/10.1007/s10578-015-0597-0 https://pubmed.ncbi.nlm.nih.gov/26493392[212] Teti DM, Kim B-R, Mayer G, Countermine M. Maternal emotional availability at bedtime predicts infant sleep quality. Journal of family psychology : JFP : journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2010;24(3):307-15
http://dx.doi.org/10.1037/a0019306 https://pubmed.ncbi.nlm.nih.gov/20545404[213] Philbrook LE, Hozella AC, Kim B-R, Jian NI, Shimizu M, Teti DM. Maternal emotional availability at bedtime and infant cortisol at 1 and 3 months. Early human development 2014;90(10):595-605
http://dx.doi.org/10.1016/j.earlhumdev.2014.05.014 https://pubmed.ncbi.nlm.nih.gov/25128871[214] Hubbard FO, Van IJzendoorn MH. Maternal unresponsiveness and infant crying across the first 9 months: A naturalistic longitudinal study Infant Behavior and Development 1991;14(3):299
[215] van IJzendoorn MH, Hubbard FO. Are infant crying and maternal responsiveness during the first year related to infant-mother attachment at 15 months? Attachment & human development 2000;2(3):371-91
https://pubmed.ncbi.nlm.nih.gov/11708224[216] Hauck YL, Hall WA, Dhaliwal SS, Bennett E, Wells G. The effectiveness of an early parenting intervention for mothers with infants with sleep and settling concerns: a prospective non-equivalent before-after design. Journal of clinical nursing 2012;21(1-2):52-62
http://dx.doi.org/10.1111/j.1365-2702.2011.03734.x https://pubmed.ncbi.nlm.nih.gov/21649763[217] Whittingham K, Douglas P. Optimizing parent-infant sleep from birth to 6 months: a new paradigm. Infant mental health journal 2014;35(6):614-23
http://dx.doi.org/10.1002/imhj.21455 https://pubmed.ncbi.nlm.nih.gov/25798510[218] Mileva-Seitz VR, Bakermans-Kranenburg MJ, Battaini C, Luijk MPCM. Parent-child bed-sharing: The good, the bad, and the burden of evidence. Sleep medicine reviews 2017;32():4-27
http://dx.doi.org/10.1016/j.smrv.2016.03.003 https://pubmed.ncbi.nlm.nih.gov/27107752[219] Volkovich E, Ben-Zion H, Karny D, Meiri G, Tikotzky L. Sleep patterns of co-sleeping and solitary sleeping infants and mothers: a longitudinal study. Sleep medicine 2015;16(11):1305-1312
http://dx.doi.org/10.1016/j.sleep.2015.08.016 https://pubmed.ncbi.nlm.nih.gov/26498228[220] Tollenaar MS, Beijers R, Jansen J, Riksen-Walraven JMA, de Weerth C. Solitary sleeping in young infants is associated with heightened cortisol reactivity to a bathing session but not to a vaccination. Psychoneuroendocrinology 2012;37(2):167-77
http://dx.doi.org/10.1016/j.psyneuen.2011.03.017 https://pubmed.ncbi.nlm.nih.gov/21530088[221] Beijers R, Riksen-Walraven JM, de Weerth C. Cortisol regulation in 12-month-old human infants: associations with the infants' early history of breastfeeding and co-sleeping. Stress (Amsterdam, Netherlands) 2013;16(3):267-77
http://dx.doi.org/10.3109/10253890.2012.742057 https://pubmed.ncbi.nlm.nih.gov/23116166[222] Waynforth D. The influence of parent-infant cosleeping, nursing, and childcare on cortisol and SIgA immunity in a sample of British children. Developmental psychobiology 2007;49(6):640-8
https://pubmed.ncbi.nlm.nih.gov/17680611[223] Lucas-Thompson R, Goldberg WA, Germo GR, Keller MA, Davis EP, Sandman CA. Sleep Arrangements and Night Waking at 6 and 12 Months in Relation to Infants' Stress-induced Cortisol Responses Infant and Child Development 2009;18(6):521
Heb je suggesties voor verbetering van deze JGZ-richtlijn?
Geef jouw feedbackLET OP: print de JGZ-richtlijn in liggende afdrukstand!
Grote tabellen zijn niet volledig zichtbaar als de JGZ-richtlijn in staande afdrukstand geprint wordt. Om kleuren in de printversie goed door te laten komen, moet bij de printerinstellingen Achtergrondillustraties aangezet worden.
Disclaimer printversie JGZ-richtlijnen
De printversie van de JGZ-richtlijn bevat de algemene tekst inclusief de aanbevelingen. De wetenschappelijke onderbouwing is terug te vinden op de website, bij de aanbevelingen onder de link “Evidence”.
