Lees meer in de onderliggende hoofdstukken.
5 Totstandkoming
JGZ-richtlijn Ondergewicht
JGZ-richtlijn Ondergewicht
Let op: deze richtlijn is momenteel in herziening.
Dit betekent niet dat de inhoud van deze richtlijn incorrect is. Tot de herziening blijft de richtlijn leidend voor de praktijk. Wel bestaat er een kans dat een deel van de informatie verouderd is.
Heb je feedback over deze JGZ-richtlijn? Stuur jouw feedback naar onze servicedesk. Zoek het tekstgedeelte waarbij je suggesties voor verbetering hebt. Via de knop ‘Geef jouw feedback’ kun je voor deze JGZ-richtlijn en het specifieke hoofdstuk jouw suggesties doorgeven.
Richtlijn inhoudsopgave
1 Inleiding Ga naar pagina over 1 Inleiding
2 Definitie en achtergrondinformatie Ga naar pagina over 2 Definitie en achtergrondinformatie
3 Signaleren, diagnostiek en verwijzen Ga naar pagina over 3 Signaleren, diagnostiek en verwijzen
4 Begeleiden en behandelen Ga naar pagina over 4 Begeleiden en behandelen
5 Totstandkoming Ga naar pagina over 5 Totstandkoming
6 Verantwoording Ga naar pagina over 6 Verantwoording
7 Bijlagen Ga naar pagina over 7 Bijlagen
1 Inleiding Ga naar pagina over 1 Inleiding
2 Definitie en achtergrondinformatie Ga naar pagina over 2 Definitie en achtergrondinformatie
3 Signaleren, diagnostiek en verwijzen Ga naar pagina over 3 Signaleren, diagnostiek en verwijzen
4 Begeleiden en behandelen Ga naar pagina over 4 Begeleiden en behandelen
5 Totstandkoming Ga naar pagina over 5 Totstandkoming
6 Verantwoording Ga naar pagina over 6 Verantwoording
7 Bijlagen Ga naar pagina over 7 Bijlagen
Heb je suggesties voor verbetering van deze JGZ-richtlijn?
Geef jouw feedbackIntroductie filmpje richtlijn Ondergewicht
PP-presentatie voor de scholing Ondergewicht
Randvoorwaardelijke implicaties richtlijn Ondergewicht
Rapportage praktijktest richtlijn Ondergewicht
BDS-registratie-protocol richtlijn Ondergewicht
Bijlage 3: Checklist anamnese en lichamelijk onderzoek
Bijlage 4: Eet en beweegdagboek 0-2 jaar
Bijlage 5: Eet en beweegdagboek 2-18 jaar
Bijlage 6: Websites bij JGZ-richtlijn Ondergewicht
Bijlage 7: Ouderinformatie ondergewicht bij jeugdigen
Bijlage 8: Tips motiverende gespreksvoering
[1] Ammaniti M, Lucarelli L, Cimino S, D'Olimpio F, Chatoor I. Feeding disorders of infancy: a longitudinal study to middle childhood. The International journal of eating disorders 2012;45(2):272-80
http://dx.doi.org/10.1002/eat.20925 https://pubmed.ncbi.nlm.nih.gov/21495054[2] Bandini LG, Anderson SE, Curtin C, Cermak S, Evans EW, Scampini R, Maslin M, Must A. Food selectivity in children with autism spectrum disorders and typically developing children. The Journal of pediatrics 2010;157(2):259-64
http://dx.doi.org/10.1016/j.jpeds.2010.02.013 https://pubmed.ncbi.nlm.nih.gov/20362301[3] Bayer O, Krüger H, von Kries R, Toschke AM. Factors associated with tracking of BMI: a meta-regression analysis on BMI tracking. Obesity (Silver Spring, Md.) 2011;19(5):1069-76
http://dx.doi.org/10.1038/oby.2010.250 https://pubmed.ncbi.nlm.nih.gov/20948517[4] Bocca-Tjeertes IFA, Kerstjens JM, Reijneveld SA, de Winter AF, Bos AF. Growth and predictors of growth restraint in moderately preterm children aged 0 to 4 years. Pediatrics 2011;128(5):e1187-94
http://dx.doi.org/10.1542/peds.2010-3781 https://pubmed.ncbi.nlm.nih.gov/21987699[5] Bryant-Waugh R, Markham L, Kreipe RE, Walsh BT. Feeding and eating disorders in childhood. The International journal of eating disorders 2010;43(2):98-111
http://dx.doi.org/10.1002/eat.20795 https://pubmed.ncbi.nlm.nih.gov/20063374[6] Dubois L, Ohm Kyvik K, Girard M, Tatone-Tokuda F, Pérusse D, Hjelmborg J, Skytthe A, Rasmussen F, Wright MJ, Lichtenstein P, Martin NG. Genetic and environmental contributions to weight, height, and BMI from birth to 19 years of age: an international study of over 12,000 twin pairs. PloS one 2012;7(2):e30153
http://dx.doi.org/10.1371/journal.pone.0030153 https://pubmed.ncbi.nlm.nih.gov/22347368[7] Dunn TM, Bratman S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eating behaviors 2016;21():11-7
http://dx.doi.org/10.1016/j.eatbeh.2015.12.006 https://pubmed.ncbi.nlm.nih.gov/26724459[8] Feldman R, Keren M, Gross-Rozval O, Tyano S. Mother-Child touch patterns in infant feeding disorders: relation to maternal, child, and environmental factors. Journal of the American Academy of Child and Adolescent Psychiatry 2004;43(9):1089-97
https://pubmed.ncbi.nlm.nih.gov/15322412[9] Herwig JE, Wirtz M, Bengel J. Depression, partnership, social support, and parenting: interaction of maternal factors with behavioral problems of the child. Journal of affective disorders 2004;80(2-3):199-208
https://pubmed.ncbi.nlm.nih.gov/15207933[10] Hulst JM, Joosten KFM. Nutrition Screening: Coding after Discharge Underestimates the Prevalence of Undernutrition. Journal of the Academy of Nutrition and Dietetics 2018;118(1):33-36
http://dx.doi.org/10.1016/j.jand.2017.05.019 https://pubmed.ncbi.nlm.nih.gov/28688884[11] Jansen PW, Roza SJ, Jaddoe VW, Mackenbach JD, Raat H, Hofman A, Verhulst FC, Tiemeier H. Children's eating behavior, feeding practices of parents and weight problems in early childhood: results from the population-based Generation R Study. The international journal of behavioral nutrition and physical activity 2012;9():130
http://dx.doi.org/10.1186/1479-5868-9-130 https://pubmed.ncbi.nlm.nih.gov/23110748[12] Johnson JG, Cohen P, Kasen S, Brook JS. Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. The American journal of psychiatry 2002;159(3):394-400
https://pubmed.ncbi.nlm.nih.gov/11870002[13] Littleton HL, Ollendick T. Negative body image and disordered eating behavior in children and adolescents: what places youth at risk and how can these problems be prevented? Clinical child and family psychology review 2003;6(1):51-66
https://pubmed.ncbi.nlm.nih.gov/12659451[14] Mader U. [Orthorexia--the addiction to nourishing oneself "healthfully"]. Deutsche medizinische Wochenschrift (1946) 2004;129(14):728
https://pubmed.ncbi.nlm.nih.gov/15104091[15] Mehta NM, Corkins MR, Lyman B, Malone A, Goday PS, Carney LN, Monczka JL, Plogsted SW, Schwenk WF, . Defining pediatric malnutrition: a paradigm shift toward etiology-related definitions. JPEN. Journal of parenteral and enteral nutrition 2013;37(4):460-81
http://dx.doi.org/10.1177/0148607113479972 https://pubmed.ncbi.nlm.nih.gov/23528324[16] O'Dea JA, Chiang H, Peralta LR. Socioeconomic patterns of overweight, obesity but not thinness persist from childhood to adolescence in a 6-year longitudinal cohort of Australian schoolchildren from 2007 to 2012. BMC public health 2014;14():222
http://dx.doi.org/10.1186/1471-2458-14-222 https://pubmed.ncbi.nlm.nih.gov/24592991[17] Pearce A, Rougeaux E, Law C. Disadvantaged children at greater relative risk of thinness (as well as obesity): a secondary data analysis of the England National Child Measurement Programme and the UK Millennium Cohort Study. International journal for equity in health 2015;14():61
http://dx.doi.org/10.1186/s12939-015-0187-6 https://pubmed.ncbi.nlm.nih.gov/26242408[18] Provost B, Crowe TK, Osbourn PL, McClain C, Skipper BJ. Mealtime behaviors of preschool children: comparison of children with autism spectrum disorder and children with typical development. Physical & occupational therapy in pediatrics 2010;30(3):220-33
http://dx.doi.org/10.3109/01942631003757669 https://pubmed.ncbi.nlm.nih.gov/20608859[19] Schönbeck Y, van Dommelen P, HiraSing RA, van Buuren S. Thinness in the era of obesity: trends in children and adolescents in The Netherlands since 1980. European journal of public health 2015;25(2):268-73
http://dx.doi.org/10.1093/eurpub/cku130 https://pubmed.ncbi.nlm.nih.gov/25125574[20] Smith S, Craig LCA, Raja EA, McNeill G, Turner SW. Prevalence and year-on-year trends in childhood thinness in a whole population study. Archives of disease in childhood 2014;99(1):58-61
http://dx.doi.org/10.1136/archdischild-2013-304423 https://pubmed.ncbi.nlm.nih.gov/24197872[21] Williams PG, Dalrymple N, Neal J. Eating habits of children with autism. Pediatric nursing 2000;26(3):259-64
https://pubmed.ncbi.nlm.nih.gov/12026389[22] Wonderlich SA, Crosby RD, Mitchell JE, Thompson KM, Redlin J, Demuth G, Smyth J, Haseltine B. Eating disturbance and sexual trauma in childhood and adulthood. The International journal of eating disorders 2001;30(4):401-12
https://pubmed.ncbi.nlm.nih.gov/11746301[23] Wright CM, Parkinson KN, Drewett RF. How does maternal and child feeding behavior relate to weight gain and failure to thrive? Data from a prospective birth cohort. Pediatrics 2006;117(4):1262-9
https://pubmed.ncbi.nlm.nih.gov/16585323[24] Wright CM, Parkinson KN, Drewett RF. The influence of maternal socioeconomic and emotional factors on infant weight gain and weight faltering (failure to thrive): data from a prospective birth cohort. Archives of disease in childhood 2006;91(4):312-7
https://pubmed.ncbi.nlm.nih.gov/16397011[25] Wright C, Birks E. Risk factors for failure to thrive: a population-based survey. Child: care, health and development 2000;26(1):5-16
https://pubmed.ncbi.nlm.nih.gov/10696514[26] Anten-Kools EJ, Wouwe JV, Oudesluys-Murphy AM, Semmekrot BA. Een professionele kijk op borstvoeding. Assen: Van Gorcum 2011
[27] Joosten K.F.M., Zwart H., Hop W.C., Hulst J.M.. Ondervoeding bij eenvijfde van kinderen opgenomen in Nederlandse ziekenhuizen. Ned Tijdschr Geneeskd. 2010;154:A1825():
[28] Joosten KFM, van Waardenberg D, Kneepkens CMF. Werkboek voeding voor zieke kinderen. Amsterdam: VU University Press 2017;ISBN:9789086597703():
http://www.stuurgroepondervoeding.nl/toolkits/werkboek-voeding-zieke-kinderen[29] Multidisciplinaire richtlijn Eetstoornissen 2006
http://www.richtlijneetstoornissen.nl[30] Oskam E., Lokven E.V., Boere-Boonekamp M.M.. Nederlands leerboek jeugdgezondheidszorg, Deel B: Inhoud (7e herz. dr.) Koninklijke Van Gorcum 2013
[31] Seys DM, Rensen JHM, Obbink MHJ. Behandelingsstrategieën bij jonge kinderen met voedings en eetproblemen. Houten (etc) Bohn, Stafleu Van Loghum 2000
[32] Van den Elzen APM, Sibbles, Drs. BJ, Nieuwenhuis, Dr. EES. Failure to thrive: van symptoom naar diagnose. Praktische pediatrie 2007;2():48
[33] American Academy of Pediatrics (2008). Recommendations for preventive pediatric health care. Pediatrics 2008;2901():
[34] Bang YK, Park MK, Ju YS, Cho KY. Clinical significance of nutritional risk screening tool for hospitalised children with acute burn injuries: a cross-sectional study. Journal of human nutrition and dietetics : the official journal of the British Dietetic Association 2018;31(3):370-378
http://dx.doi.org/10.1111/jhn.12518 https://pubmed.ncbi.nlm.nih.gov/28948659[35] Becker PJ, Nieman Carney L, Corkins MR, Monczka J, Smith E, Smith SE, Spear BA, White JV. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition). Journal of the Academy of Nutrition and Dietetics 2014;114(12):1988-2000
http://dx.doi.org/10.1016/j.jand.2014.08.026 https://pubmed.ncbi.nlm.nih.gov/25458748[36] Brener ND, Mcmanus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 2003;32(4):281-7
https://pubmed.ncbi.nlm.nih.gov/12667732[37] Chourdakis M, Hecht C, Gerasimidis K, Joosten KF, Karagiozoglou-Lampoudi T, Koetse HA, Ksiazyk J, Lazea C, Shamir R, Szajewska H, Koletzko B, Hulst JM. Malnutrition risk in hospitalized children: use of 3 screening tools in a large European population. The American journal of clinical nutrition 2016;103(5):1301-10
http://dx.doi.org/10.3945/ajcn.115.110700 https://pubmed.ncbi.nlm.nih.gov/27099244[38] Elia M, Stratton RJ. Considerations for screening tool selection and role of predictive and concurrent validity. Current opinion in clinical nutrition and metabolic care 2011;14(5):425-33
http://dx.doi.org/10.1097/MCO.0b013e328348ef51 https://pubmed.ncbi.nlm.nih.gov/21832898[39] Erkan T. Methods to evaluate the nutrition risk in hospitalized patients. Turk pediatri arsivi 2014;49(4):276-81
http://dx.doi.org/10.5152/tpa.2014.2226 https://pubmed.ncbi.nlm.nih.gov/26078678[40] Hartman C, Shamir R, Hecht C, Koletzko B. Malnutrition screening tools for hospitalized children. Current opinion in clinical nutrition and metabolic care 2012;15(3):303-9
http://dx.doi.org/10.1097/MCO.0b013e328352dcd4 https://pubmed.ncbi.nlm.nih.gov/22588189[41] Himes JH, Faricy A. Validity and reliability of self-reported stature and weight of US adolescents. American journal of human biology : the official journal of the Human Biology Council 2001;13(2):255-60
https://pubmed.ncbi.nlm.nih.gov/11460871[42] Hulst JM, Zwart H, Hop WC, Joosten KFM. Dutch national survey to test the STRONGkids nutritional risk screening tool in hospitalized children. Clinical nutrition (Edinburgh, Scotland) 2010;29(1):106-11
http://dx.doi.org/10.1016/j.clnu.2009.07.006 https://pubmed.ncbi.nlm.nih.gov/19682776[43] Huybrechts I, Himes JH, Ottevaere C, De Vriendt T, De Keyzer W, Cox B, Van Trimpont I, De Bacquer D, De Henauw S. Validity of parent-reported weight and height of preschool children measured at home or estimated without home measurement: a validation study. BMC pediatrics 2011;11():63
http://dx.doi.org/10.1186/1471-2431-11-63 https://pubmed.ncbi.nlm.nih.gov/21736757[44] Huysentruyt K, Alliet P, Muyshont L, Rossignol R, Devreker T, Bontems P, Dejonckheere J, Vandenplas Y, De Schepper J. The STRONG(kids) nutritional screening tool in hospitalized children: a validation study. Nutrition (Burbank, Los Angeles County, Calif.) 2013;29(11-12):1356-61
http://dx.doi.org/10.1016/j.nut.2013.05.008 https://pubmed.ncbi.nlm.nih.gov/24103513[45] Jensen NSO, Camargo TFB, Bergamaschi DP. Comparison of methods to measure body fat in 7-to-10-year-old children: a systematic review. Public health 2016;133():3-13
http://dx.doi.org/10.1016/j.puhe.2015.11.025 https://pubmed.ncbi.nlm.nih.gov/26774698[46] Joosten KFM, Hulst JM. Prevalence of malnutrition in pediatric hospital patients. Current opinion in pediatrics 2008;20(5):590-6
http://dx.doi.org/10.1097/MOP.0b013e32830c6ede https://pubmed.ncbi.nlm.nih.gov/18781124[47] Joosten KFM, Hulst JM. Nutritional screening tools for hospitalized children: methodological considerations. Clinical nutrition (Edinburgh, Scotland) 2014;33(1):1-5
http://dx.doi.org/10.1016/j.clnu.2013.08.002 https://pubmed.ncbi.nlm.nih.gov/24050847[48] Kyle UG, Earthman CP, Pichard C, Coss-Bu JA. Body composition during growth in children: limitations and perspectives of bioelectrical impedance analysis. European journal of clinical nutrition 2015;69(12):1298-305
http://dx.doi.org/10.1038/ejcn.2015.86 https://pubmed.ncbi.nlm.nih.gov/26039314[49] Ling R.E., Hedges V., Sullivan P.B.. Nutritional risk in hospitalised children: An assessment of two instruments e-SPEN, the European e-Journal of Clinical Nutrition and Metabolism 2011;6(3):
[50] Moeeni V, Walls T, Day AS. The STRONGkids nutritional risk screening tool can be used by paediatric nurses to identify hospitalised children at risk. Acta paediatrica (Oslo, Norway : 1992) 2014;103(12):e528-31
http://dx.doi.org/10.1111/apa.12768 https://pubmed.ncbi.nlm.nih.gov/25130603[51] Novianti D., Sembiring T., Sofyani S., Faranita T., Pratita W.. Screening for nutritional risk in hospitalized children: comparison of two instruments Paediatrica Indonesiana 2017;57(3):117
[52] de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization 2007;85(9):660-7
https://pubmed.ncbi.nlm.nih.gov/18026621[53] Peng L-T, Li R, Zhao W-H, Chen Y-H, Li X-M, Chen M-Y, Cao J, Li X-N. [Nutritional risk screening and its clinical significance in 706 children hospitalized in the surgical department]. Zhongguo dang dai er ke za zhi = Chinese journal of contemporary pediatrics 2013;15(10):880-5
https://pubmed.ncbi.nlm.nih.gov/24131842[54] Reilly HM, Martineau JK, Moran A, Kennedy H. Nutritional screening--evaluation and implementation of a simple Nutrition Risk Score. Clinical nutrition (Edinburgh, Scotland) 1995;14(5):269-73
https://pubmed.ncbi.nlm.nih.gov/16843942[55] Rinninella E, Ruggiero A, Maurizi P, Triarico S, Cintoni M, Mele MC. Clinical tools to assess nutritional risk and malnutrition in hospitalized children and adolescents. European review for medical and pharmacological sciences 2017;21(11):2690-2701
https://pubmed.ncbi.nlm.nih.gov/28678315[56] Scherdel P, Dunkel L, van Dommelen P, Goulet O, Salaün J-F, Brauner R, Heude B, Chalumeau M. Growth monitoring as an early detection tool: a systematic review. The lancet. Diabetes & endocrinology 2016;4(5):447-56
http://dx.doi.org/10.1016/S2213-8587(15)00392-7 https://pubmed.ncbi.nlm.nih.gov/26777129[57] Silva AM, Fields DA, Sardinha LB. A PRISMA-driven systematic review of predictive equations for assessing fat and fat-free mass in healthy children and adolescents using multicomponent molecular models as the reference method. Journal of obesity 2013;2013():148696
http://dx.doi.org/10.1155/2013/148696 https://pubmed.ncbi.nlm.nih.gov/23844282[58] Silveira J., Pinho J.. MON-PP157: Adaptation of an Evaluation Tool for Nutritional Risk in a Pediatric Service Clinical Nutrition 2015;34, S186():
[59] Teixeira AF, Viana KDAL. Nutritional screening in hospitalized pediatric patients: a systematic review. Jornal de pediatria 2016;92(4):343-52
http://dx.doi.org/10.1016/j.jped.2015.08.011 https://pubmed.ncbi.nlm.nih.gov/26859247[60] Vegelin AL, Brukx LJCE, Waelkens JJ, Van den Broeck J. Influence of knowledge, training and experience of observers on the reliability of anthropometric measurements in children. Annals of human biology 2003;30(1):65-79
https://pubmed.ncbi.nlm.nih.gov/12519655[61] Wells JCK, Fewtrell MS. Measuring body composition. Archives of disease in childhood 2006;91(7):612-7
https://pubmed.ncbi.nlm.nih.gov/16790722[62] White M, Lawson K, Ramsey R, Dennis N, Hutchinson Z, Soh XY, Matsuyama M, Doolan A, Todd A, Elliott A, Bell K, Littlewood R. Simple Nutrition Screening Tool for Pediatric Inpatients. JPEN. Journal of parenteral and enteral nutrition 2016;40(3):392-8
http://dx.doi.org/10.1177/0148607114544321 https://pubmed.ncbi.nlm.nih.gov/25096546[63] de Wilde JA, van Dommelen P, Middelkoop BJC. Appropriate body mass index cut-offs to determine thinness, overweight and obesity in South Asian children in the Netherlands. PloS one 2013;8(12):e82822
http://dx.doi.org/10.1371/journal.pone.0082822 https://pubmed.ncbi.nlm.nih.gov/24367559[64] de Wilde JA, van Dommelen P, van Buuren S, Middelkoop BJC. Height of South Asian children in the Netherlands aged 0-20 years: secular trends and comparisons with current Asian Indian, Dutch and WHO references. Annals of human biology 2015;42(1):38-44
http://dx.doi.org/10.3109/03014460.2014.926988 https://pubmed.ncbi.nlm.nih.gov/24963814[65] . WHO Child Growth Standards based on length/height, weight and age. Acta paediatrica (Oslo, Norway : 1992). Supplement 2006;450():76-85
https://pubmed.ncbi.nlm.nih.gov/16817681[66] Wiskin AE, Owens DR, Cornelius VR, Wootton SA, Beattie RM. Paediatric nutrition risk scores in clinical practice: children with inflammatory bowel disease. Journal of human nutrition and dietetics : the official journal of the British Dietetic Association 2012;25(4):319-22
http://dx.doi.org/10.1111/j.1365-277X.2012.01254.x https://pubmed.ncbi.nlm.nih.gov/22591201[67] Wonoputri N, Djais JTB, Rosalina I. Validity of nutritional screening tools for hospitalized children. Journal of nutrition and metabolism 2014;2014():143649
http://dx.doi.org/10.1155/2014/143649 https://pubmed.ncbi.nlm.nih.gov/25298890[68] Becker P, Carney LN, Corkins MR, Monczka J, Smith E, Smith SE, Spear BA, White JV, , . Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition). Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition 2015;30(1):147-61
http://dx.doi.org/10.1177/0884533614557642 https://pubmed.ncbi.nlm.nih.gov/25422273[69] Briggs-Gowan M.J., Carter A.S., Irwin J.R., Wachtel K., Cicchetti D.V.. Brief Infant-Toddler Social and Emotional Assessment (BITSEA) Manual, Version 2.0 2002
[70] Hendrikse WH, Reilly JJ, Weaver LT. Malnutrition in a children's hospital Clin. Nutr. 1997;16():13
[71] Hulst J, Joosten K, Zimmermann L, Hop W, van Buuren S, Büller H, Tibboel D, van Goudoever J. Malnutrition in critically ill children: from admission to 6 months after discharge. Clinical nutrition (Edinburgh, Scotland) 2004;23(2):223-32
https://pubmed.ncbi.nlm.nih.gov/15030962[72] Van Heerwaarden Y. Aansluiten bij ouders van vandaag. Samen met ouders een passende route uitstippelen voor de ondersteuning van kinderen bij het opgroeien en opvoeden. NCJ - Nederlands Centrum Jeugdgezondheid, Utrecht 2012
https://www.NCJ.nl[73] Van Heerwaarden Y, Pijpers F. De kracht van zelfregie. Samen komen tot passende hulp en ondersteuning. NCJ - Nederlands Centrum Jeugdgezondheid, Utrecht 2015
https://www.NCJ.nl[74] Goodman R. The Strengths and Difficulties Questionnaire: a research note. Journal of child psychology and psychiatry, and allied disciplines 1997;38(5):581-6
https://pubmed.ncbi.nlm.nih.gov/9255702[75] Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. The British journal of psychiatry : the journal of mental science 2000;177():534-9
https://pubmed.ncbi.nlm.nih.gov/11102329[76] NVK. Richtlijn Ondergewicht 2019
https://www.NVK.nl[77] Olsen EM. Failure to thrive: still a problem of definition. Clinical pediatrics 2006;45(1):1-6
https://pubmed.ncbi.nlm.nih.gov/16429209[78] Olsen EM, Petersen J, Skovgaard AM, Weile B, Jørgensen T, Wright CM. Failure to thrive: the prevalence and concurrence of anthropometric criteria in a general infant population. Archives of disease in childhood 2007;92(2):109-14
https://pubmed.ncbi.nlm.nih.gov/16531456[79] WHO. Management of severe malnutrition: a manual for physicians and other senior health workers. Geneva: World Health Organization 1999
[80] Schönbeck Y, Talma H, van Dommelen P, Bakker B, Buitendijk SE, Hirasing RA, van Buuren S. Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PloS one 2011;6(11):e27608
http://dx.doi.org/10.1371/journal.pone.0027608 https://pubmed.ncbi.nlm.nih.gov/22110687[81] Chatoor I, Ganiban J, Colin V, Plummer N, Harmon RJ. Attachment and feeding problems: a reexamination of nonorganic failure to thrive and attachment insecurity. Journal of the American Academy of Child and Adolescent Psychiatry 1998;37(11):1217-24
https://pubmed.ncbi.nlm.nih.gov/9808934[82] Florence MD, Asbridge M, Veugelers PJ. Diet quality and academic performance. The Journal of school health 2008;78(4):209-15; quiz 239-41
http://dx.doi.org/10.1111/j.1746-1561.2008.00288.x https://pubmed.ncbi.nlm.nih.gov/18336680[83] French SA, Stables G. Environmental interventions to promote vegetable and fruit consumption among youth in school settings. Preventive medicine 2003;37(6 Pt 1):593-610
https://pubmed.ncbi.nlm.nih.gov/14636793[84] Hofman E.. Kleine eters: peuters en kleuters met eetproblemen. Amsterdam: Boom 2006
[85] Hoyland A, Lawton CL, Dye L. Acute effects of macronutrient manipulations on cognitive test performance in healthy young adults: a systematic research review. Neuroscience and biobehavioral reviews 2008;32(1):72-85
https://pubmed.ncbi.nlm.nih.gov/17629947[86] iReasearch. Evaluatieonderzoek De Gezonde Schoolkantine 2010
[87] Perry CL, Bishop DB, Taylor GL, Davis M, Story M, Gray C, Bishop SC, Mays RAW, Lytle LA, Harnack L. A randomized school trial of environmental strategies to encourage fruit and vegetable consumption among children. Health education & behavior : the official publication of the Society for Public Health Education 2004;31(1):65-76
https://pubmed.ncbi.nlm.nih.gov/14768658[88] Taras H. Nutrition and student performance at school. The Journal of school health 2005;75(6):199-213
https://pubmed.ncbi.nlm.nih.gov/16014126[89] Van den Engel-Hoek L, van Gerven M, de Groot S, van Haaften L, van Hulst K. Eet- en drinkproblemen bij jonge kinderen (4 ed.). Assen: Van Gorcum 2011
[90] Williams KE, Field DG, Seiverling L. Food refusal in children: a review of the literature. Research in developmental disabilities 2010;31(3):625-33
http://dx.doi.org/10.1016/j.ridd.2010.01.001 https://pubmed.ncbi.nlm.nih.gov/20153948[91] de Wit J. Lichamelijke gevolgen van eetstoornissen bij kinderen. In: Messer AP, Vos I de, Wolters WHG. Eetproblemen bij kinderen en adolescenten. Baarn: Ambo 1994
[92] Argumentenfabriek. Knelpuntenanalyses jeugdgezondheidszorg. 2015
1 Inleiding
Deze richtlijn is bedoeld voor JGZ-professionals (dit zijn jeugdartsen, verpleegkundig specialisten*, jeugdverpleegkundigen, doktersassistenten) en beoogt richtinggevend te zijn bij het handelen tijdens contacten met individuele 0-18 jarigen en hun ouders/verzorgers.
De richtlijn ‘Ondergewicht’ beschrijft het normale gewichtsverloop en de begrippen ondergewicht en ondervoeding en geeft handelingsaanbevelingen ten behoeve van:
- het monitoren van het gewicht en het signaleren van ondergewicht en ondervoeding;
- het verwijzen bij ondergewicht en/of een afbuigende gewichtscurve;
- de advisering bij ondergewicht.
In de richtlijn worden vragen van JGZ-professionals beantwoord. Deze vragen werden voorafgaand aan de ontwikkeling geprioriteerd en geformuleerd tijdens een knelpuntenanalyse onder leiding van de Argumentenfabriek [92]. Een projectgroep van TNO schreef de teksten voor de richtlijn geschreven in samenwerking met een werkgroep met vertegenwoordigers van JGZ-professionals, ouders en diverse andere experts (zie ook sectie Totstandkoming). De teksten zijn mede beoordeeld door een klankbordgroep en door professionals en andere belanghebbenden tijdens een landelijke commentaarronde. Vier JGZ-organisaties hebben de richtlijn in de praktijk getest.
Op 4 maart 2019 heeft de Richtlijn Adviescommissie (RAC) de richtlijn geautoriseerd. De RAC heeft bij haar beoordeling rekening gehouden met de inhoud van de richtlijn (wetenschappelijke onderbouwing, opzet) en de voor implementatie vereiste randvoorwaarden. Parallel aan de ontwikkeling van deze richtlijn voor JGZ-professionals heeft de Nederlandse Vereniging voor Kindergeneeskunde (NVK) een richtlijn geschreven over de diagnostiek, behandeling en follow-up bij kinderen en adolescenten met ondergewicht en/of een afbuigende gewichtscurve. Op de punten waar de richtlijnen overlappen of op elkaar aansluiten heeft afstemming plaatsgevonden.
*De verpleegkundig specialist preventieve zorg is een verpleegkundige met een BIG geregistreerde masteropleiding die werkzaamheden van het medisch domein combineert met die van het verpleegkundig domein binnen het eigen deskundigheidsgebied en zij werkt op expertniveau. Zij is binnen dit expertisegebied o.a. bevoegd om zelfstandig te werken, diagnoses te stellen en te verwijzen waar nodig is. De verpleegkundig specialist is lid van het JGZ team, zij maakt net als de andere teamleden gebruik van de expertise van collega’s en speciaal van de jeugdarts als het gaat om complexe medische problematiek.
1.1 Afbakening
De JGZ-richtlijn ‘Ondergewicht’ is ontwikkeld op basis van de knelpuntenanalyse, zoals deze is uitgevoerd door het CBO & de Argumentenfabriek [92]. Bij de knelpuntenanalyse waren diverse JGZ-professionals betrokken. De aldaar geformuleerde uitgangsvragen zijn beantwoord:
- Welke kennis, vaardigheden en instrumenten moeten JGZ-professionals inzetten om ondergewicht door voeding (ondervoeding) of door systemische, psychosociale of somatische oorzaken bij kinderen tijdig te signaleren en juist te volgen?
- Op welke alarmsignalen bij ondergewicht van kinderen moeten JGZ-professionals letten (herkennen/signaleren) om tijdig door te verwijzen of te behandelen en welk instrument kunnen ze hiervoor gebruiken?
- Welke adviezen over voeding en risicofactoren kunnen JGZ-professionals geven aan ouders van en kinderen met een verhoogd risico op ondergewicht?
- Welke verwijscriteria moeten JGZ-professionals gebruiken voor doorverwijzing om ondergewicht tijdig en passend te laten behandelen?
De JGZ-richtlijn ‘Ondergewicht’ sluit met name aan bij de JGZ-richtlijnen:
2 Definitie en achtergrondinformatie
Onderstaande tekst is gebaseerd op handboeken [30][31], overzichtsartikelen [15][32], andere richtlijnen (met name de JGZ-richtlijn ‘Voeding en eetgedrag’ , de NVK richtlijn ‘Voedingsgedrag bij kinderen’ en de ‘Multidisciplinaire richtlijn Eetstoornissen’ van het CBO), informatie van het Voedingscentrum.
Voor informatie over het onderwerp lengtegroei verwijzen we naar de gelijknamige JGZ-richtlijn.
2.1 Kernpunten
- Gewicht en lengte zijn voor een groot deel familiair bepaald en sterk gerelateerd aan afkomst.
- Bij een gewicht dat beduidend lager is dan gebruikelijk voor jeugdigen van dezelfde lichaamslengte en/of leeftijd wordt gesproken van ondergewicht.
- Een jeugdige met ondergewicht kan ondervoed zijn, maar dat hoeft niet. Als de jeugdige zijn/haar gewichtscurve blijft volgen en het gewicht niet afbuigt, is deze misschien licht voor zijn leeftijd en/of lichaamslengte maar is er geen reden tot zorg.
- Ondervoeding is een toestand waarbij een structurele disbalans bestaat tussen voedingsbehoefte en voedselinname, waardoor toenemende tekorten aan energie, eiwit en andere voedingsstoffen, met meetbaar nadelige effecten op vorm en functie van de weefsels en het lichaam, op groei en ontwikkeling en op de klinische uitkomsten van ziekte.
- Ondervoeding kan ontstaan doordat een kind te weinig of te selectief eet en/of veel energie en voedingsstoffen verbruikt of verliest.
- Vroeggeboorte, voedingsproblemen, ernstige eetproblemen, (beginnende) eetstoornissen en ziekte zijn belangrijke risicofactoren voor ondergewicht en ondervoeding.
2.2 Normale groei
2.2.1 Baby’s
In Nederland bedraagt het geboortegewicht bij jongens gemiddeld 3.482 gram bij een gemiddelde lengte van 51 cm, bij meisjes is dit 3.374 gram en 50 cm (bron: CBS-statline). Meisjes zijn bij geboorte en daarna gemiddeld lichter dan jongens. Kinderen van Zuidoost-Aziatische afkomst − waaronder Hindostaanse kinderen*− zijn door hun lichaamsbouw lichter dan kinderen van Nederlandse afkomst.
In het eerste halfjaar na de geboorte zijn kinderen die voornamelijk moedermelk krijgen gemiddeld iets zwaarder dan kinderen die vooral kunstvoeding krijgen. Vanaf de derde of vierde levensmaand neemt het gewicht van kinderen die moedermelk krijgen minder snel toe (in de volksmond ook wel ‘4 maanden dip’ genoemd). Dit is een normaal verschijnsel. In het tweede halfjaar na de geboorte is het omgekeerd: kinderen die kunstvoeding krijgen zijn over het algemeen wat zwaarder [26]. Verschillen door het soort voeding zijn meestal rond het tweede levensjaar verdwenen. Zie verder: multidisciplinaire richtlijn Borstvoeding.
Een speciale groep wordt gevormd door de vroeg (prematuur) geboren kinderen. Veel van deze kinderen zijn niet alleen vroeg geboren maar hebben ook een intra-uteriene groeiachterstand (d.w.z. ze zijn small for gestational age (SGA)/dysmatuur) (zie ook JGZ-richtlijn ‘Vroeg en/of Small voor Gestational Age (SGA) geboren kinderen’). Zij vertonen in de eerste levensjaren vaker een laag gewicht dan op tijd geboren kinderen.
Gewicht, maar ook lengte en BMI, zijn voor een groot deel familiair bepaald. Het effect van genetische factoren is laag bij geboorte maar neemt daarna snel toe. Vanaf de leeftijd van vijf maanden wordt 80-90% van de variantie door genetische factoren verklaard [6].
Met de groei veranderen ook de lichaamsverhoudingen. Door de relatief korte armen en benen krijgt de babyromp extra nadruk. Door toename van het onderhuidse vet lijkt een baby tussen 3-9 maanden ‘dik’ of ‘mollig’ met een ‘rond’ lijfje en ‘ronde’ benen en armen. Dit verdwijnt weer in de peuterperiode.
*deze term wordt in Nederland en in Suriname vaak gebruikt om de bevolkingsgroep aan te duiden die van Indiase of Zuid-Aziatische afkomst is
2.2.2 Peuters en basisschoolkinderen
Bij gezonde, jonge kinderen komt het voor dat gedurende de eerste twee levensjaren een relatieve versnelling of vertraging van de groei optreedt. Vanaf twee jaar verloopt de groei van het gewicht en de lengte dan minder snel en gaat elk kind zijn/haar eigen, individuele curve volgen. Kinderen met een lage (of hoge) BMI op deze leeftijd hebben een verhoogde kans om later ook een lage (of hoge) BMI te hebben [3].
Veel kinderen zijn een periode selectief bij het eten of eten minder. Dit hoort bij de normale ontwikkeling maar kan bijvoorbeeld ook gebeuren bij een belangrijke ontwikkelingsstap of bij een ingrijpende gebeurtenis. Ook tijdens en na een ziekteperiode of ziekenhuisopname kunnen kinderen sterk wisselen in wat en hoeveel ze eten. Doorgaans gaat dit gedrag vanzelf over en is er weinig effect op de voedingstoestand van het kind. Voor meer informatie en aanbevelingen, zie de JGZ-richtlijn ‘Voeding en eetgedrag’.
2.2.3 Puberteit
In de puberteit maakt het lichaam een groeispurt door en vindt er een karakteristieke verandering in lichaamsverhoudingen plaats. In de eerste fase van de groei zijn het vooral de armen en benen die verhoudingsgewijs lang worden, pas later groeit de romp. Ook de voeten maken een vroege groeispurt door, maar stoppen al weer snel. Veranderingen in de breedte van schouders en bekken ontstaan nog weer later. Het lichaamsgewicht neemt vlak voor en tijdens de puberteit sterk toe. Het gewicht wordt in de adolescentieperiode zelfs bijna verdubbeld.
In de prepuberteit neemt bij jongens en meisjes de vetafzetting toe. Daarna is de gewichtstoename voornamelijk het gevolg van de groei van vetvrije massa (skelet, spieren, organen en dergelijke). Bij jongens neemt de spiermassa beduidend meer toe dan bij meisjes. Jongens kunnen in de periode van maximale groei zelfs vet verliezen. Bij meisjes neemt aan het einde van de puberteit de vetmassa lokaal weer duidelijk toe.
2.3 Ondergewicht en ondervoeding
2.3.1 Definitie
Ondergewicht
Bij een gewicht dat lager is dan gebruikelijk voor jeugdigen van dezelfde lichaamslengte en/of leeftijd wordt gesproken van ondergewicht. In deze richtlijn wordt gesproken van ondergewicht bij een gewicht-naar-leeftijd of een gewicht-naar-lengte < -2 SDS of een BMI-naar-leeftijd corresponderend met een BMI < 17,0 kg/m2 op leeftijd van 18 jaar. Een jeugdige met ondergewicht kan ondervoed zijn, maar dat hoeft niet. Er kan ook sprake zijn van een constitutioneel of familiair laag gewicht. Als de jeugdige zijn/haar gewichtscurve blijft volgen en het gewicht niet afbuigt, is de jeugdige misschien licht voor de leeftijd en/of lichaamslengte maar is er geen reden tot zorg. Stagnatie van de groei of ongewild in korte tijd veel afvallen is een ongunstiger teken.
Ondervoeding
Figuur 1.1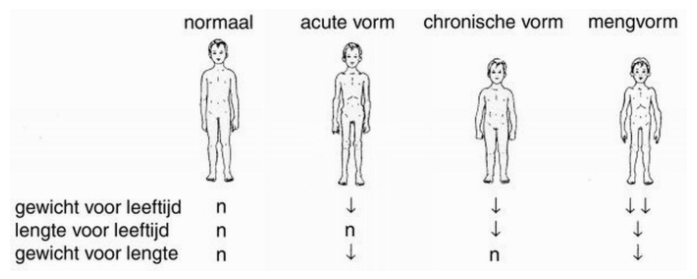
De Nederlandse Vereniging voor Kindergeneeskunde (NVK) definieert ondervoeding als een toestand waarbij een disbalans bestaat tussen voedingsbehoefte en voedselinname, waardoor toenemende tekorten aan energie, eiwit en andere voedingstoffen ontstaan, met meetbaar nadelige effecten op vorm en functie van de weefsels en het lichaam, op groei en ontwikkeling en op de klinische uitkomstmaten van ziekte.
De disbalans die bij ondervoeding bestaat tussen voedingsbehoefte en voedselinname kan vele oorzaken hebben (zie subsectie Oorzaken Tabel 2.1). Kinderartsen en kinderverpleegkundigen onderscheiden acute en chronische ondervoeding. Bij acute ondervoeding wordt vooral gewichtsverlies gezien dat optreedt door een veranderde stofwisseling, een verminderde voedselinname en braken en/of diarree door acute ziekte. Bij acute ondervoeding daalt het gewicht, maar is de lengtegroei (nog) niet achtergebleven. Er is dus sprake van een laag gewicht voor de lengte (in Engelstalige literatuur aangeduid als ‘wasting’).
Bij chronische ondervoeding is niet alleen het gewicht aangedaan, maar blijft ook de lengtegroei achter (in Engelstalige literatuur: ‘stunting’). Chronische ondervoeding kan optreden bij chronische ziekte of bij langdurige eetproblemen. Behalve de ziekte zelf kan ook de behandeling van de ziekte invloed hebben op de voedingstoestand en op de groei. Zo is één van de mogelijke bijwerkingen van het gebruik van methylfenidaat bij ADHD of autisme het verlies van eetlust en verminderde groei. Zie ook de JGZ-richtlijn ‘Lengtegroei’.
Bij een kind kan ook sprake zijn van zowel acute áls chronische ondervoeding. Dit wordt gemengde ondervoeding genoemd.
2.3.2 Epidemiologie
Ondergewicht
Uit de CBS gezondheidsenquête uit 2017 komt naar voren dat 7,7% van de 4 tot 12 jarigen en 3,3% van de 12 tot 18 jarigen ondergewicht heeft.
De Nederlandse groeistudie [19] geeft ook cijfers over het aantal kinderen in Nederland met ondergewicht. Voor deze studie werden de groeigegevens van 54.814 Nederlandse kinderen in de leeftijd van 2-18 jaar gemeten vanaf 1980 tot en met 2009. Als afkapwaarde voor het ondergewicht namen de onderzoekers de voor leeftijd en geslacht specifieke BMI die correspondeert met een BMI van 17,0 op 18 jarige leeftijd. Volgens deze definitie had in 2009 9,8% van de jongens en meisjes van Nederlands afkomst ondergewicht. Voor kinderen en adolescenten van Turkse afkomst was dit 5,7% en voor kinderen en adolescenten van Marokkaanse afkomst 6,2%. Ondergewicht kwam het meest voor bij kinderen in de leeftijd van 2-5 jaar, gevolgd door de leeftijdscategorie 12-19 jaar.
De literatuur is niet eensluidend over de relatie tussen sociale klasse en ondergewicht. Onderzoek in Groot-Brittannië liet zien dat kinderen in de lagere sociale klassen een licht verhoogde kans hebben op ondergewicht [17]. Andere onderzoekers, uit Schotland en Australië, konden dit niet bevestigen [20][16].
Ondervoeding
Er zijn geen actuele gegevens over hoe vaak ondervoeding in Nederland bij jeugdigen voorkomt. Er zijn wel gegevens over het aantal ondervoede kinderen bij opname in een ziekenhuis. Vanaf 2008 worden alle kinderen die >24 uur in het ziekenhuis worden opgenomen (dat zijn 80-100.000 kinderen per jaar) gescreend op acute ondervoeding. In 2015 was bij 6,5% van hen sprake van acute ondervoeding [10].
2.3.3 Oorzaken
Er zijn veel verschillende oorzaken mogelijk voor ondergewicht en ondervoeding. Voor een overzicht (zie Tabel 2.1). De voor JGZ-professionals belangrijkste risicofactoren worden hieronder beschreven.
Tabel 2.1: Overzicht mogelijke oorzaken voor ondergewicht en ondervoeding [32][15][6][28](JGZ-richtlijn ‘Voeding en eetgedrag’)
|
Familiair/constitutioneel
|
Toegenomen energiebehoefte/verhoogd metabolisme Gedrag
Infectie
Trauma
Oncologisch
Hart
Longen
Nieren
Abdomen
Bloed
Endocrinologie
Neurologie
Metabool
Perinataal
|
|
Inadequate inname Voedingsproblemen
Eetproblemen/-stoornissen
Slik/eetproblemen door somatische factoren
Psychosociaal
|
|
|
Overmatig verlies/inadequate verwerking Diarree
Braken
|
Vroeg- en/of SGA geboorte
Vroeg geboren kinderen laten in de eerste levensjaren vaker een groeiachterstand zien. Het wat lagere gewicht is meestal geen punt van zorg en wordt veelal in de loop van de eerste levensjaren ingehaald [4]. Met name SGA geboren kinderen hebben een verhoogd risico op het niet inhalen van deze achterstand (JGZ-richtlijn ‘Vroeg en/of Small voor Gestational Age (SGA) geboren kinderen’).
Voedings- en eetproblemen [25][23]
Bij zuigelingen kunnen problemen bij borstvoeding, verkeerd bereide kunstvoeding, slecht drinken, weinig zuigkracht, langzaam drinken of een vertraagde overgang van melkvoeding op vaste voeding tot ondergewicht en een achterblijvende groei leiden (Edmond 2007).
Bij 25% tot 45% van de gezonde peuters en kleuters komen lichte tot matige voeding- en eetproblemen (bijvoorbeeld weinig eten, selectief eten, afwijzen van onbekende producten) voor. Deze kinderen groeien en functioneren meestal goed. Bij kinderen met een psychomotorische retardatie of kinderen met een chronische ziekte komen voeding- en eetproblemen veel vaker voor (40-80%) en zijn deze ernstiger. Vroeg geborenen kinderen, kinderen of adolescenten met een langdurige ziekenhuisopname, kinderen die op jonge leeftijd ernstig ziek zijn geweest en kinderen die om medische redenen langdurig sondevoeding hebben gehad, hebben door de negatieve ervaringen een verhoogd risico op het ontwikkelen van een eetprobleem met extreem vermijdingsgedrag [76].
Psychosociale factoren kunnen bijdragen aan het ontstaan of het in stand houden van eetproblemen. Eetgedrag heeft op elke leeftijd een signaalfunctie: eetgedrag kan een mogelijkheid zijn voor een kind om zijn/haar emoties te uiten, zeker als het kind nog niet beschikt over de cognitieve of verbale mogelijkheden om emoties te uiten. Maar ook bij oudere kinderen en tieners kan het eetgedrag het eerste signaal zijn dat de jeugdige ‘niet goed in zijn/haar vel’ zit. Kinderen met internaliserende (angst, depressie) en externaliserende problemen (druk gedrag en hyperactiviteit) hebben vaker eetproblemen, wat op termijn kan leiden tot ondergewicht [18][21][31]. Uit de literatuur komt verder naar voren dat opvoedingsproblemen [11][13], problemen in de ouder-kind relatie [8], verwaarlozing [9], en mishandeling [12][22] bij kunnen dragen aan het ontstaan van ondergewicht, meestal doordat het kind door middel van eetproblemen de ervaren stress uit. Ook kinderen van wie de ouders psychiatrische problemen hebben, ervaren vaker dan andere kinderen psychosociale problemen en zijn extra gevoelig voor het ontwikkelen van eetproblemen [5][1].
Ook somatische aspecten kunnen aanleiding zijn voor eetproblemen. Zo lijdt volgens tandartsen naar schatting tien procent van de Nederlandse kinderen onder de vijf jaar aan ernstige cariës. Een slechte mondgezondheid kan door pijn, ontstekingen en abcessen serieuze gevolgen hebben voor onder meer het eetpatroon. Ook bij obstipatie kunnen door buikpijn, een verminderde eetlust en ‘discomfort’ eetproblemen ontstaan. Somatische factoren waarbij sprake is van slikproblematiek en/of waarbij de eetlust is verminderd zijn bijvoorbeeld: een strakke tongriem, adenotonsillaire hypertrofie, mond motorische dysfunctie, chronische ernstige dyspnoe, gastro-oesofageale reflux en voedselallergie of -overgevoeligheid.
Kinderen met overgewicht kunnen ondervoed raken terwijl zij veel eten, maar niet genoeg gezonde voedingsstoffen binnenkrijgen. Denk bijvoorbeeld aan het overmatig eten van producten met veel suiker, zout en vet waardoor er tekorten ontstaan aan andere voedingsstoffen. Ook het volgen van een extreem of langdurig dieet kan tot ondervoeding leiden.
Extreem selectief eetgedrag kan voedingsdeficiënties veroorzaken. Extreem selectieve eters weigeren specifieke voeding met een bepaalde smaak, geur of structuur; hun weigergedrag gaat verder dan de angst die veel jonge kinderen vertonen voor onbekende voedingsmiddelen. Kinderen met dit soort problemen kunnen ook op andere sensorische gebieden overgevoelig zijn (geluidsprikkels, vieze handen). Extreem selectief eetgedrag komt relatief vaak voor bij kinderen met Autisme Spectrum Stoornis (ASS) [2].
Bij extreem en dwangmatig gezond eten (ook wel aangeduid als ‘orthorexia’) worden steeds meer soorten voeding uit het menu geschrapt, vooral voedingsmiddelen die relatief veel calorieën, vet of suikers bevatten, ook wel in combinatie met extreem veel sporten. Jeugdigen en volwassenen die geobsedeerd raken door gezonde voedingsmiddelen lopen het risico om deze obsessie door te ontwikkelen naar een eetstoornis, vooral in combinatie met psychologische risicofactoren zoals een negatief zelfbeeld en de sterke wens om slank te zijn [14][29][7]. Orthorexia wordt door kinder- en jeugdpsychiaters en psychologen wel gezien als een voorstadium van anorexia. Hoe vaak orthorexia bij jeugdigen voorkomt is niet bekend.
Eetstoornissen
Anorexia nervosa leidt tot significant ondergewicht en ondervoeding. Anorexia komt met name voor bij meisjes en jonge vrouwen in de leeftijd van 9-19 jaar. De ‘life-time’ prevalentie wordt voor meisjes en vrouwen op 1-4% geschat, voor jongens en mannen op 0,3-0,7%. Tot nu toe is geen enkele opzichzelfstaande etiologische factor geïdentificeerd als dé veroorzaker, maar een belangrijke psychische risicofactor is een negatieve lichaamsbeleving. Specifieke risicogroepen voor het ontwikkelen van een eetstoornis zijn fotomodellen in de modewereld, balletdansers en topsporters [29].
Ziekte
Ziekte is een belangrijke oorzaak voor ondergewicht en ondervoeding. Van den Elzen (2007) maakt grofweg onderscheid in ziekten die leiden tot of gepaard gaan met:
- Onvoldoende inname van energie en eiwit (bijvoorbeeld door ernstige cariës, dyspneu);
- Toegenomen energiebehoefte ( bijvoorbeeld bij recidiverende (KNO) infecties, langdurige koorts, een hartafwijking)
- Verhoogd verlies van voedingstoffen (door braken en/of diarree zoals bijvoorbeeld bij gastro-enteritis, voedselallergie, actieve coeliakie of inflammatoire darmziekten) [32].
2.3.4 Gevolgen
Korte termijn
Ondervoeding kan ernstige gevolgen hebben voor de gezondheid en het welbevinden van jeugdigen (Tabel 2.2). Directe lichamelijke gevolgen zijn afvallen, lage bloedsuikerspiegel (hypoglykemie), verlies van spiermassa (en op basis daarvan verminderde spierkracht, moeheid) en verhoogde vatbaarheid voor infecties [15]. Het langdurig niet eten van één of meer voedingsmiddelen of het op grond van bepaalde overtuigingen aanpassen van het voedingspatroon zonder dit te compenseren door gelijkwaardige producten kan voedingsdeficiënties (bijvoorbeeld ijzer, calcium) veroorzaken. Sommige gevolgen van ondervoeding kunnen levensbedreigend zijn, zoals hartritmestoornissen, decompensatio cordis of hypoglykemie.
Psychische klachten bij ondervoeding kunnen zijn: depressiviteit, (sociale) angstklachten, gedragsproblemen, concentratie- en geheugenstoornissen, obsessief denken over eten. Ondervoeding leidt tot een langzamer herstel en complicaties bij ziekte en operaties. Kinderen met acute ondervoeding verblijven gemiddeld 45% langer in het ziekenhuis dan kinderen met een normale voedingstoestand [27].
Tabel 2.2: Korte- en langetermijngevolgen van ondervoeding [91][27][29](Colbert 2004)
| Korte termijn |
|
| Lange termijn |
|
Lange termijn
Ondervoeding kan leiden tot een vertraagde groei en ontwikkeling [15]. Meestal buigt dan eerst het gewicht en later de lengte af [91]. Bij kinderen jonger dan twee jaar kan ook de schedelgroei achterblijven [15]. Bij normalisering van het onvolwaardige voedingspatroon treedt inhaalgroei op. Maar het eerdere groeiniveau wordt niet altijd meer bereikt. Groeiachterstand kan ook leiden tot een achterstand in de cognitieve ontwikkeling (Colbert 2004). Kinderen met een groeiachterstand hebben vaker een achterstand in de taalontwikkeling en gedragsproblemen [15]. Bij oudere kinderen kan ondervoeding leiden tot het uitblijven van de menstruatie en de seksuele rijping, zie verder de JGZ-richtlijn ‘Seksuele ontwikkeling’ of de JGZ-richtlijn ‘Lengtegroei’.
3 Signaleren, diagnostiek en verwijzen
Tot de taken van JGZ-professionals behoren onder meer het monitoren van de groei en het signaleren van ondergewicht. Ondergewicht is een belangrijke indicator voor ondervoeding en kan wijzen op de aanwezigheid van een somatische of niet-somatische ziekte of probleem. Hieronder worden handelingsaanbevelingen rondom dit thema gegeven; d.w.z. hoe bij jeugdigen met ondergewicht of een afbuigende gewichtscurve beoordeeld kan worden of verdere actie (verwijzing, begeleiding) is aangewezen.
De uitvoering en interpretatie van gewicht- en lengtemetingen worden beschreven in Bijlage 1 van deze richtlijn. Afkappunten voor ondergewicht en een afbuigende gewichtscurve staan in subsectie Criteria ondergewicht/afbuigende gewichtscurve.
Criteria voor achterblijvende lengtegroei worden gegeven in de JGZ-richtlijn ‘Lengtegroei’.
3.1 Lichaamsmetingen
Aanbevelingen
3.2 Groeidiagrammen
Aanbevelingen
3.3 Criteria ondergewicht/afbuigende gewichtscurve
In de JGZ wordt van ondergewicht gesproken als er sprake is van een gewicht naar leeftijd/lengte <-2 SDS of een BMI naar leeftijd die correspondeert met een BMI van <17,0 kg/m2 op 18 jaar. Van een afbuigende gewichtscurve is sprake als de SD score sinds de vorige meting met >1 SD afgenomen.
3.4 Extra onderzoek door de JGZ
Bij zorgen over het gewicht of het gewichtsverloop wordt met behulp van het JGZ-dossier en een gerichte voedingsanamnese in combinatie met een medische anamnese en lichamelijk onderzoek het risico op ondervoeding onderzocht om te bepalen of verdere actie (begeleiding, verwijzing) nodig is. Mogelijke onderliggende oorzaken worden bespreekbaar gemaakt. In Bijlage 3 staat een lijst die kan hierbij helpen. In overleg met de ouder(s) en/of de jeugdige kan hiervoor een extra consult op indicatie worden ingepland.
Het ontwikkelingsniveau van de jeugdige wordt door de JGZ-professional op de gebruikelijke wijze onderzocht met behulp van het JGZ-dossier, het Van Wiechenonderzoek, de Baecke-Fassaert-motoriektest en de puberteitsstadia. De SDQ (Strength and Difficulties Questionnaire; [74][75]), of voor jongere kinderen de BITSEA (Brief Infant-Toddler Social and Emotional Assessment; [69]), kunnen wijzen op het bestaan van psychosociale problematiek.
Als hulpmiddel bij de voedingsanamnese kunnen de ouders voor kinderen ouder dan vier jaar (of de jeugdige zelf) de Eetmeter van het Voedingscentrum invullen en meenemen bij het bezoek aan de JGZ. Zie de website van het Voedingcentrum Mijn.voedingscentrum.nl. Bespreek met ouders of het hen lukt om dit te doen. Zo nodig kan een papieren dagboekje meegegeven worden (zie Bijlagen 4 en 5).
Inschatten voedingstoestand
De JGZ-professional schat de voedingstoestand van de jeugdige in door middel van het meten en volgen van het gewicht en de lengte (zie sectie Signaleren, diagnostiek en verwijzen) maar bij geconstateerd ondergewicht en/of een afbuigende gewichtscurve vooral ook door de klinische blik. De klinische blik geeft de doorslag of verwijzing is aangewezen of niet.
Aspecten die kunnen wijzen op ondervoeding:
- Ingevallen gelaat
- Verminderde hoeveelheid subcutaan vet, gewichtsverlies
- Verminderde spiermassa
- Het kind is apathisch, moe, passief
- Slappe handdruk, verminderde spierkracht
- Conditie van de huid is verminderd, de huid is droog, schilferig, bleek
- Conditie van het haar is verslechterd, dof haar
- Zieke indruk
- Vertraagde schedelgroei (<2 jaar)
- Stilstand in de lengtegroei, zie JGZ-richtlijn ‘Lengtegroei’
- Ontwikkelingsniveau
- Gedragsproblemen
- Bij oudere kinderen: uitblijvende menstruatie, vertraagde seksuele of puberteitsontwikkeling
Risico op ondervoeding
De JGZ-professional is bij kinderen met ondergewicht en/of een afbuigende gewichtscurve alert op mogelijke oorzaken voor de achterstand, zie subsectie Oorzaken.
Bij zuigelingen kunnen voedingsproblemen (borstvoeding ‘loopt niet goed’, complicaties bij borstvoeding), verkeerd bereide kunstvoeding (te weinig schepjes of juist te veel), slecht drinken, weinig zuigkracht, langzaam drinken of een vertraagde overgang van melkvoeding op vaste voeding tot dehydratie en ondervoeding leiden.
Ook langdurende en ernstige eetproblemen (dat wil zeggen voedselweigering > 1 maand of extreem selectief eetgedrag) en (beginnende) eetstoornissen leiden tot een verhoogd risico op ondervoeding. Milde eetproblemen (bijvoorbeeld minder eten, selectief eten, afwijzen van onbekende producten) komen weliswaar veel voor maar gaan in de meeste gevallen vanzelf over en hebben weinig effect op de voedingstoestand. Bij kinderen vanaf de leeftijd van ongeveer negen jaar is de JGZ-professional alert op (beginnende) anorexia nervosa. Voor meer informatie over eetstoornissen en kenmerken van ernstige eetproblemen, zie JGZ-richtlijn ‘Voeding en eetgedrag’ .
Er kan ook een hoog risico op ondervoeding bestaan op grond van de aanwezigheid van een somatische ziekte of – probleem. Ziekten en problemen met een hoog risico op ondervoeding (in alfabetische volgorde; [42]) staan genoemd in Tabel 4.1.
Tabel 4.1 Ziekten en problemen met een hoog risico op ondervoeding [42]
|
|
|
|
Verdenking op een (ernstige) onderliggende ziekte of – probleem
Ondergewicht en/of een afbuigende gewichtscurve kunnen in de praktijk, meestal in combinatie met andere symptomen of klachten, ook een eerste uiting zijn van een (tot dan toe onontdekte) onderliggende ziekte of – probleem:
- Ondergewicht in combinatie met mond sensomotorische problemen (zoals verslikken na iedere voeding, overmatig kwijlen) en persisterende slik- en/of voedingspassageklachten (>1 week) kan wijzen op een neurologische – of ontwikkelingsstoornis.
- Ondergewicht in combinatie met frequent braken kan passen bij een anatomische afwijking van het maagdarmkanaal (o.a. oesofagusatresie, ziekte van Hirschsprung) of een syndromale aandoening, verhoogde hersendruk (door bijvoorbeeld een hersentumor of hydrocephalus), een metabole ziekte of een eetstoornis. Differentiaal diagnostisch is hierbij ook de aard van het braken (zelfopgewekt of niet), het tijdstip van braken (’s ochtends, in aansluiting of vlak na het eten) en het aspect van het braaksel (gallig braken, stinkend braken, bloedbraken) van belang.
- Bij een kind met ondergewicht en een afwijkend defecatiepatroon, zoals diarree, ontkleurde ontlasting en bloed bij de ontlasting, kan sprake zijn van malabsorptie (bijvoorbeeld door koemelkeiwitallergie, coeliakie, infectie met Giardia Lamblia, cystic fibrosis of een inflammatoire darmziekte).
Aanbevelingen
3.5 Verwijzen
Jeugdigen met ondergewicht en/of een afbuigende gewichtscurve worden naar een kinderarts verwezen als:
- Er naar inschatting van de jeugdarts of de verpleegkundig specialist sprake is van een afwijkende voedingstoestand en/of een verhoogd risico op ondervoeding;
- Er in de medische anamnese tevens sprake is van klachten of symptomen die kunnen wijzen op een (ernstige) onderliggende ziekte of – probleem;
- Begeleiding vanuit de JGZ en/of het inschakelen van een (kinder)diëtist niet voldoende helpt, er bij de professional of de ouder(s) zorgen blijven bestaan of als de voedingstoestand verder verslechtert.
Verwijzing naar een kinderarts gaat gepaard met bericht aan de huisarts. Een (standaard) begeleidende brief en een kopie van de verwijsbrief worden na toestemming van de ouders naar de huisarts gestuurd. In de verwijsbrief staan de adresgegevens van zowel de verwijzer (de jeugdarts of de verpleegkundig specialist) als de huisarts vermeld en de ontvanger wordt verzocht naar beide beroepsgroepen terug te rapporteren. In de verwijsbrief wordt ten minste de SD score van het gewicht-naar-leeftijd/lengte en het gewichtsverloop (als mate van afname van de SD score) genoemd.
Jeugdigen die voor verwijzing al behandeld werden door bijvoorbeeld een (kinder)diëtist blijven daar ook na de verwijzing onder behandeling. Wanneer bij een jeugdige met ondergewicht verwijzing naar een andere professional dan de kinderarts ook of meer van toepassing is kan de jeugdarts, de verpleegkundig specialist en/of de jeugdverpleegkundige daar (in overleg met de ouders en de jeugdige) voor kiezen:
- (Kinder)diëtist. Voor het in kaart brengen en beoordelen van het voedingspatroon, voor begeleiding bij het bereiken van een normaal gewicht en voor het normaliseren van het voedingspatroon en het eetgedrag kan verwezen worden naar een (kinder)diëtist. Een (kinder)diëtist kan jeugdigen met ondergewicht, een afbuigende groeicurve of een onvolwaardig of ongebalanceerde voedingsinname en hun ouders begeleiden en advies op maat geven. Doel is om het gewicht en het voedingspatroon te normaliseren. Bij selectieve en/of restrictieve eters kan de (kinder)diëtist bijvoorbeeld beoordelen of er sprake is van een volwaardige en gebalanceerd voedingsinname en advies geven over energie- en eiwitrijke voeding of over de inzet van dieetvoeding.
- Pedagoog/ gedragstherapeut. Bij vragen over het eetgedrag en de ouder-kind interactie en als er veel pedagogische problemen rondom het eten zijn of een negatieve interactie tussen ouders en de jeugdige en als advisering vanuit de JGZ onvoldoende helpt, is het raadzaam om hulp van een pedagoog/ gedragstherapeut in te schakelen.
- Preverbaal logopedist. Voedingsproblemen moeten altijd in relatie tot de totale ontwikkeling worden gezien. Leren eten van een lepel, drinken uit een fles, beker of rietje en kauwen op vast voedsel zijn motorische vaardigheden die moeten aansluiten bij het motorisch functioneren van het kind. Bij problemen met het drinken uit de borst of uit de fles, het eten van de lepel, het drinken uit een beker, het leren kauwen en/of het slikken kan verwijzing naar een preverbaal logopedist aangewezen zijn. Preverbaal logopedisten zijn gespecialiseerd in slikproblemen en eet- en drinkproblemen bij jonge kinderen.
- Lactatiekundige. Bij problemen bij borstvoeding kan worden verwezen naar een lactatiekundige. Voor een gezonde groei is het advies dat baby’s op verzoek borstvoeding krijgen. Dit houdt in: zo vaak en lang als het kind wil, zowel overdag als ’s nachts. In de eerste levensweek betekent dit minimaal acht voedingen per etmaal. Vanaf het moment dat het kind meer bijvoeding krijgt, drinkt het minder en neemt de hoeveelheid moedermelk af. Kolven van moedermelk kan noodzakelijk zijn om de melkproductie op gang te brengen of te houden, bijvoorbeeld als de moeder weer gaat werken (zie verder ‘Multidisciplinaire richtlijn borstvoeding’ ).
- KNO-arts. Bij voornamelijk KNO-problemen.
- Huisarts.Verwijzing naar de huisarts kan van toepassing zijn bij problemen in de gezinscontext of in de directe leefomgeving, bij vragen over de medische voorgeschiedenis of bij psychosociale problemen. Ook een sociaal wijkteam kan ingezet worden (indien beschikbaar). Er kan ook gekozen worden om verwijzing naar de kinderarts via de huisarts te laten verlopen, bijvoorbeeld voor (extra) motivatie om een verwijzing op te volgen.
- Eerstelijns eetteams. Voor multidisciplinaire begeleiding bij voedings- en eetproblemen zijn in verschillende regio’s en gemeenten eerstelijns eetteams actief. Hierin wordt samengewerkt door o.a. een (kinder)diëtist, een preverbaal logopedist, een kinderergotherapeut, een pedagoog/kinderpsycholoog en een kinderfysiotherapeut. Soms is ook een kinderarts aangesloten. Voor een overzicht, zie Bijlage 6.
Aanbevelingen
4 Begeleiden en behandelen
4.1 Voorlichting
Een deel van de jeugdigen heeft van ‘nature’ een lager gewicht dan de meeste leeftijdsgenoten van hetzelfde geslacht en lengte. Er is dan sprake van familiair of constitutioneel ondergewicht. Hieraan wordt met name gedacht als één of beide biologische ouders een lage BMI hebben of als het kind prematuur of SGA geboren is. Ook kan het gewicht van vooral jongens door de groeispurt in de puberteit (tijdelijk) laag zijn. Als de jeugdige weliswaar ondergewicht heeft maar zijn/haar curve blijft volgen, er geen zorgen zijn over het eten en hij/zij goed gezond is en goed functioneert is in principe geen verdere actie nodig. De JGZ blijft de groei op de gebruikelijke wijze volgen (zie sectie Signaleren, diagnostiek en verwijzen). Op verzoek kan de jeugdarts of de verpleegkundig specialist uitleg geven over de normale ontwikkeling en fase problematiek. Eventuele preventieve voedingsadvisering is gericht op het in stand houden van een gezond voedingspatroon en het behouden van een voor de betreffende jeugdige gezond gewicht.
Aanbevelingen
4.2 Begeleiden
Aan (ouders van) jeugdigen met ondergewicht waarbij sprake is van een mild, mogelijk voorbijgaand voedings- of eetprobleem dat weinig effect heeft op de voedingstoestand én er geen klachten of symptomen zijn die kunnen duiden op een onderliggende, ernstige ziekte of een (beginnende) eetstoornis wordt begeleiding aangeboden.
Voorwaarde voor het succesvol begeleiden van jeugdigen met ondergewicht en/of een afbuigende groeicurve is dat het probleem door de jeugdigen en zijn/haar ouders/verzorgers wordt onderkend zodat zij openstaan voor adviezen. In Bijlage 8 worden tips voor motiverende gespreksvoering gegeven. Voor algemene informatie en praktische aanbevelingen, zie de NCJ handreiking ‘Aansluiten bij ouders van vandaag’ [72] (http://www.ncj.nl). Wijzen op de informatie op de website van het Voedingscentrum kan ook helpen. De huisarts kan worden ingeschakeld om de jeugdige en zijn/haar ouders/verzorgers (extra) te motiveren, bijvoorbeeld om verwijzing naar een kinderarts op te volgen. Ouders vinden het verder belangrijk dat de JGZ de groei van hun kind bijhoudt. Ze doen dat vaak zelf ook, meestal met behulp van een app.
Doel van de begeleiding is het bereiken van een volwaardige en gebalanceerde voedingsinname, leeftijdsadequaat eetgedrag en een voor de betreffende jeugdige gezond gewicht. Om dit doel te bereiken kan de hulp van een (kinder)diëtist of een pedagoog/gedragstherapeut nodig zijn. Ook kan overwogen worden om een lactatiekundige, een preverbaal logopedist, de huisarts of een eerstelijns eetteam in te schakelen.
Voor de begeleiding van jeugdigen met ondergewicht en/of een afbuigende gewichtscurve en hun ouders kunnen zo nodig enkele extra contacten op indicatie ingepland worden, voor advisering op maat. Onderwerpen voor advisering kunnen zijn: de normale ontwikkeling en fase problematiek, gezonde voeding en leeftijdsadequaat eetgedrag, omgaan met eetproblemen en opvoedproblemen rondom eten (zie JGZ-richtlijn ‘Voeding en eetgedrag’ en Adviseren ). De aard en inhoud van de begeleiding, en ook het aantal en de frequentie van de extra contacten, is afhankelijk van onder andere de leeftijd van het kind en de complexheid en de aard van de (vermoedelijke) problematiek. Enkele extra meet- en weegmomenten kunnen worden afgesproken voor evaluatie van de ingezette begeleiding. Als de achterstand in gewicht niet (voldoende) wordt ingehaald kan de jeugdarts of de verpleegkundig specialist alsnog besluiten te verwijzen naar een kinderarts.
Aanbevelingen
4.3 Adviseren
In dit thema wordt ingegaan op de advisering bij ondergewicht of een neerwaarts afbuigende gewichtscurve. De inhoud van dit thema is grotendeels gebaseerd op de JGZ-richtlijn ‘Voeding en eetgedrag’.
Aanbevelingen
4.3.1 Adviezen 0 – 1 jaar
Adviezen aan jeugdigen met ondergewicht en hun ouders zijn gericht op het bereiken en/of in stand houden van een volwaardige en gebalanceerde inname van voedingsstoffen conform de Schijf van Vijf. De basis voor een gezonde voeding en een gezond voedingspatroon staat omschreven in de JGZ-richtlijn ‘Voeding en eetgedrag’.
Basisadviezen zijn:
- Hanteren van vaste eet- en drinkmomenten;
- Aandacht voor adequate intake van smeer- en bereidingsvet;
- Adequate intake van zuivel en drinken water/thee;
- Beperken inname van suikerhoudende dranken;
- Tijdige opbouw van vaste voeding na de periode van melkvoeding;
- De aanbevolen hoeveelheid aan inname van voedingsstoffen wordt uit alle vakken van de Schijf van Vijf gehaald (ook voor kinderen met ondergewicht is voeding met veel verzadigd vet en/of suiker ongezond!)
Adviezen 0 – 1 jaar
Bij het introduceren van nieuwe voedingsmiddelen wordt aanbevolen om deze af te wisselen en vaker aan te bieden. Wijs ouders erop dat nieuwe voedingsmiddelen tenminste tien keer of vaker aan het kind moeten worden aangeboden zodat het aan de nieuwe smaak kan wennen. Daarnaast dient er variatie aan voedingsmiddelen te worden geadviseerd. De ouders bepalen wat het kind eet, maar het kind geeft de hoeveelheden aan. De voeding en het eetgedrag moeten passen bij het ontwikkelingsniveau van het kind (knoeien mag!).
Aanbevelingen voorlichting 0 – 1 jaar
De JGZ richtlijn ‘Voeding en Eetgedrag’ geeft aanbevelingen ten aanzien van de voorlichting aan ouders van kinderen in de leeftijd van 0-1 jaar:
- Door het zo jong mogelijk aanleren van gezonde voedingsgewoonten en adequaat eetgedrag wordt de basis gelegd voor een gezond voedingspatroon op latere leeftijd. Het is belangrijk dat ouders en kind in het eerste levensjaar een ontspannen voedingsinteractie opbouwen. Door responsief te reageren op signalen van honger en verzadiging, leert het kind de juiste verbanden te leggen, namelijk dat honger leidt tot het aanbieden van voeding, – en dat verzadiging; stoppen met voeden – samengaat met tevredenheid en ontspanning. Responsief opvoedgedrag ondersteunt het kind om zijn/haar eigen lichaam en voedingsbehoeften te leren kennen. Dit draagt ook bij aan de ontwikkeling van een veilige hechting [81].
- Voorkomen moet worden dat het voeden vergezeld gaat van externe controle of dat er veel druk uitgeoefend wordt bij het eten, bijvoorbeeld door strakke regels te hanteren, voeding op te dringen, of eten te geven voor oneigenlijke doeleinden, zoals troost of compensatie.
- Ouders wordt geadviseerd om te letten op signalen van honger en verzadiging bij hun kind. Signalen van honger bij een baby zijn minder diepe slaap, zoekgedrag, zuigen op de handjes, bewegen met het mondje en uiteindelijk huilen. Bij verzadiging laat een baby meestal de tepel of speen van de fles los. Andere signalen van verzadiging zijn zich strekken, kokhalzen of het hoofd wegdraaien [89]. Vooral bij volledige zuigelingenvoeding is het belangrijk dat ouders weten dat het niet nodig is om altijd de hele fles leeg te laten drinken.
‘Eetplezier en Beweegkriebels’ (http://www.voedingscentrum.nl/eetplezier) is een ouderworkshop over het belang van gezonde voeding en voldoende bewegen. Het kan door kinderopvang, buurthuizen of in de JGZ ingezet worden om ouders te helpen bij het aanleren van een gezonde leefstijl bij hun kinderen. De interventie is goed onderbouwd.
‘Smakelijke Eters’ (http://www.voedingscentrum.nl/webshop) is een workshop voor ouders van kinderen in de leeftijd van 0-4 jaar om hen te helpen hun kinderen duurzaam gezonde eetgewoonten bij te brengen. De interventie werd door het RIVM Centrum Gezond Leven (CGL) aangemerkt als ‘goed onderbouwd’.
Verwijzen
Als advisering door de JGZ niet haalbaar en/of niet effectief is, dan is verwijzing naar een (kinder)diëtist voor een dieetadvies op maat of naar een pedagoog/gedragstherapeut voor hulp bij opvoedingsproblemen raadzaam.
4.3.2 Adviezen 1 – 4 jaar
Adviezen aan jeugdigen met ondergewicht en hun ouders zijn gericht op het bereiken en/of in stand houden van een volwaardige en gebalanceerde inname van voedingsstoffen conform de Schijf van Vijf. De basis voor een gezonde voeding en een gezond voedingspatroon staat omschreven in de JGZ-richtlijn ‘Voeding en eetgedrag’.
Basisadviezen zijn:
- Hanteren van vaste eet- en drinkmomenten;
- Aandacht voor adequate intake van smeer- en bereidingsvet;
- Adequate intake van zuivel en drinken water/thee;
- Beperken inname van suikerhoudende dranken;
- Tijdige opbouw van vaste voeding na de periode van melkvoeding;
- De aanbevolen hoeveelheid aan inname van voedingsstoffen wordt uit alle vakken van de Schijf van Vijf gehaald (ook voor kinderen met ondergewicht is voeding met veel verzadigd vet en/of suiker ongezond!)
Adviezen 1 – 4 jaar
Tussen de maaltijden door kan er geadviseerd worden om een extra boterham, fruit of yoghurt te eten. Snoep, snacks en suikerhoudende dranken zijn ook voor kinderen met ondergewicht ongezond.
De aanbevolen hoeveelheden van een voedingsmiddelengroep staat weergegeven in Bijlagen 2 en 3 van de JGZ-richtlijn ‘Voeding en eetgedrag’. Daarnaast is het advies aan ouders om een goede basisvoorraad boodschappen in huis te hebben zodat er altijd iets te eten is, ook voor tussendoor.
Aan ouders wordt uitgelegd dat om te beoordelen of een kind genoeg eet, goede groei en goed functioneren de belangrijkste parameter is. Wat en hoeveel een kind eet zijn dan van secundair belang. Bij gezonde jonge kinderen vormen voedingsovergangen, ziekteperioden en belangrijke ontwikkelingssprongen of levensgebeurtenissen kwetsbare momenten voor het ontstaan van eetproblemen [84].
Mee eten met de ouders en eventuele andere gezinsleden heeft over het algemeen een positieve invloed op het aanleren van gezond eetgedrag. Een jong kind eet de ene keer minder, maar compenseert dit in de regel een andere keer weer. Kinderen zullen zichzelf niet snel uithongeren. De behoefte aan voedsel neemt af in de peutertijd omdat de groeisnelheid trager is dan die van zuigelingen. Het opdringen van eten kan leiden tot verzet en angst bij het kind, en tevens overgewicht stimuleren. Ook een te permissieve opvoedstijl (onder andere weghalen van ongewenst voedsel, het aanbieden van een geliefder alternatief) is niet effectief: er zijn positieve samenhangen gevonden met eetproblemen, en slechtere uitkomsten voor voeding en gewicht [90].
Bij de ontwikkeling van eetgedrag spelen leerprocessen een rol. Kinderen leren door ervaring en imitatie. Eetgedrag dat vooraf wordt gegaan door positieve prikkels (ontspannen sfeer, lekkere geur) of dat positieve gevolgen heeft (prettige smaakervaring, verzadigd gevoel, compliment) zal zich eerder herhalen dan eetgedrag dat plaatsvindt onder fysiek onaangename (kokhalzen, verslikken) of stressvolle condities en/of dat pijn, spanning of straf veroorzaakt. Een kind zal producten die positieve associaties oproepen opnieuw willen verkrijgen, terwijl negatieve associaties vermijding of voedselweigering in de hand werken [31].
Opvoedingsadviezen 1 – 4 jaar
In de JGZ-richtlijn ‘Voeding- en eetgedrag’ worden opvoedingsadviezen voor ouders van kinderen in de leeftijd van 1-4 jaar gegeven:
- Bouw een herkenbaar eetritme op door op een vaste plaats, bijvoorbeeld aan tafel, en op vaste tijden te eten.
- Bied het kind maximaal zeven eet- en drinkmomenten aan per dag; geef hongergevoel een kans.
- Beperk omgevingsprikkels, zet bijvoorbeeld de televisie uit.
- Geef ‘s avonds of ‘s nachts in bed geen eten of drinken, behalve water.
- Gebruik geen afleidingsmanoeuvres om het kind te laten eten.
- Geef een kind voldoende tijd om nieuwe smaken te leren kennen. Kook geen aparte maaltijden.
- Gebruik geen eten om een bepaald gedrag te stimuleren (belonen) of juist te ontmoedigen (straffen)
- Weigergedrag moet zoveel mogelijk worden genegeerd. Zet het kind zo nodig kort op een time-outplek. Voorkom dwingend voeden. Achtervolg het kind niet met voeding. Ook uithongeren, dreigen of straffen en apart laten eten zijn niet effectief. Forceren is niet effectief en kan leiden tot negatieve associaties rond eten zoals angst en verzet.
- Voorkom mechanistisch voeden op de klok, zonder rekening te houden met de signalen van het kind.
- Als eten tijdelijk niet lukt, richt de aandacht dan op andere activiteiten met het kind die wel soepel verlopen. Zo blijft de band goed.
- Stimuleer dat het kind voldoende beweegt binnen en bij voorkeur ook buitenshuis: buiten spelen en veel bewegen wekt een hongergevoel op.
- Ga bij verandering van eetgedrag na of het kind ergens mee zit of iets onder de leden heeft.
- Streef als ouder naar voldoende rust en ontspanning voor uzelf. Voorkom overbelasting en schakel op tijd hulp in. Hoe eerder een eetprobleem wordt opgelost, hoe beter.
en adviezen ten aanzien van het gezamenlijk eten (aan tafel):
- Eet samen met het kind en geef zelf het goede voorbeeld.
- Zorg voor een ontspannen, vriendelijke sfeer. Stress vermindert de eetlust.
- Bied ruimte voor ontwikkeling en het opdoen van ervaring. Knoeien hoort erbij. Bepaal als ouders wel de grenzen.
- Neem een ondersteunende en stimulerende houding aan en focus op wat goed gaat. Dit geeft het kind zelfvertrouwen, en houdt de sfeer goed.
- Presenteer de maaltijd uitnodigend en betrek het kind eventueel bij het klaarmaken en opscheppen ervan.
- Spreek als ouders met elkaar tafelregels af en geef het kind het voorbeeld met een korte en duidelijke uitleg.
- Bepaal als ouders samen de aanpak en steun elkaar in de uitvoering ervan. Vermijd conflicten aan tafel.
- Neem voldoende tijd om te eten. 20-30 minuten aan tafel zitten is voor de meeste kinderen voldoende.
- Haal na de maaltijd het bord weg; het volgende vaste eet en/of drinkmoment biedt de eerste nieuwe kans voor het kind om weer te eten. Biedt dus geen alternatieven aan, ook als het kind weinig gegeten heeft.
Verwijzen
Als advisering door de JGZ niet haalbaar en/of niet effectief is, dan is verwijzing naar een (kinder)diëtist voor een dieetadvies op maat of naar een pedagoog/gedragstherapeut voor hulp bij opvoedingsproblemen raadzaam.
4.3.3 Adviezen 5 – 18 jaar
Adviezen aan jeugdigen met ondergewicht en hun ouders zijn gericht op het bereiken en/of in stand houden van een volwaardige en gebalanceerde inname van voedingsstoffen conform de Schijf van Vijf. De basis voor een gezonde voeding en een gezond voedingspatroon staat omschreven in de JGZ-richtlijn ‘Voeding en eetgedrag’
Basisadviezen zijn:
- Hanteren van vaste eet- en drinkmomenten;
- Aandacht voor adequate intake van smeer- en bereidingsvet;
- Adequate intake van zuivel en drinken water/thee;
- Beperken inname van suikerhoudende dranken;
- Tijdige opbouw van vaste voeding na de periode van melkvoeding;
- De aanbevolen hoeveelheid aan inname van voedingsstoffen wordt uit alle vakken van de Schijf van Vijf gehaald (ook voor kinderen met ondergewicht is voeding met veel verzadigd vet en/of suiker ongezond!)
Adviezen 5 -18 jaar
Het bijhouden van een eetdagboek kan ouders en professionals helpen inzicht in de voedingsinname van de jeugdige te krijgen. Voor kinderen ouder dan vier jaar kunnen ouders (of de jeugdige zelf) de Eetmeter van het Voedingscentrum invullen en meenemen bij het bezoek aan de JGZ: https://mijn.voedingscentrum.nl/ . Eventueel kan een papieren dagboek meegegeven worden (zie Bijlagen 4 en 5).
Tussen de maaltijden door kan er geadviseerd worden om een extra boterham, fruit of yoghurt te eten. Snoep, snacks en suikerhoudende dranken zijn ook voor kinderen met ondergewicht ongezond.
De aanbevolen hoeveelheden van een voedingsmiddelengroep staat weergegeven in Bijlagen 2 en 3 van de JGZ-richtlijn ‘Voeding en eetgedrag’. Daarnaast is het advies aan ouders om een goede basisvoorraad boodschappen in huis te hebben zodat er altijd iets te eten is, ook voor tussendoor.
Kinderen in de groei hebben vaak grotere porties nodig. Dit geldt voornamelijk als zij hier ook veel bij bewegen.
De pedagogische advisering en de aanbevolen hoeveelheden, zoals beschreven in subsectie Adviezen 1 – 4 jaar, blijven hetzelfde.
Aandachtspunten
Aandachtspunten genoemd in de JGZ-richtlijn ‘Voeding en eetgedrag’ voor het ontwikkelen van een gezond en goed eetgedrag bij schoolkinderen en jongeren zijn:
Rol van ouders en leeftijdsgenoten. Voor jonge kinderen zijn de ouders (en verzorgers) het belangrijkste voorbeeld voor eet- en beweeggedrag. De invloed van leeftijdsgenoten neemt met het stijgen van de leeftijd toe. Daarom is het voor ouders van belang om hun kinderen al vroeg bij te brengen dat gezonde voeding belangrijk is. Het eetpatroon en inkoopbeleid van de ouders zijn factoren die meewegen in de voedingskeuzes die jongeren zelf gaan maken. Uit onderzoek blijkt verder dat hoe vaker ouders samen eten met hun pubers, hoe gezonder hun eetgedrag is.
Bij migrantengezinnen is het van belang te weten dat ook andere volwassenen dan de ouders in de ‘extended family’ een rolmodel zijn voor het eetgedrag. Bovendien kan eten een grotere sociale functie hebben dan de Nederlandse eettafel.
Rol van school. ‘Smaaklessen’ is een lesprogramma over voeding voor groep 1 t/m 8 van de basisschool (zie verder http://webshop.voedingscentrum.nl/smaaklessen.html ). Door te proeven, ruiken, horen, voelen en kijken verkennen kinderen hun eten. ‘Smaakplezier’ voor op de buitenschoolse opvang sluit hierbij aan.
Jongeren schaffen gezondere voedingsproducten aan wanneer ze aangeboden worden [83][87]. Onderzoek heeft laten zien dat een gezonder aanbod van voeding op school leidt tot gezonder eetgedrag van jongeren. Het programma ‘De Gezonde Schoolkantine’ van het Voedingscentrum zorgt voor een beter aanbod [86] (http://www.voedingscentrum.nl/gezondeschoolkantine). Er zijn aanwijzingen dat de kwaliteit van de voeding in positieve zin samenhangt met cognitieve ontwikkeling en schoolprestaties van jongeren [82][88][85][91]. De interventie wordt aangemerkt als goed onderbouwd.
Rol van de (sociale) media. Voor jongeren zijn (sociale) media belangrijk. De media verschaffen zeer veel, maar ook tegenstrijdige informatie over wat gezonde voeding is. Onderzoek van het Voedingscentrum laat zien dat met name de groep jong volwassenen (tussen 18 en 29 jaar) regelmatig in verwarring is na gesprekken over gezonde voeding. Ongeveer de helft van deze groep zoekt wekelijks naar informatie over voeding. Het is daarom aan te bevelen om ouders en kinderen te wijzen op websites waar betrouwbare informatie te vinden is over voeding en eetgedrag zoals van het Voedingscentrum (http://www.voedingscentrum.nl/nl/mijn-kind-en-ik.aspx)
Rol van lijnen en een negatief zelfbeeld. Naarmate kinderen ouder worden, wordt uiterlijk belangrijker. Kinderen met een gezond gewicht kunnen al op 9- tot 10-jarige leeftijd een negatief zelfbeeld hebben. Er kan dan ook al sprake van lijngedrag zijn. Vooral meisjes willen graag slank zijn en beginnen met lijnen. Letten op de lijn kan gezond zijn met het oog op preventie van overgewicht en obesitas, maar extreem lijngedrag dient beslist voorkomen te worden omdat dit een verhoogd risico inhoudt om een eetstoornis te ontwikkelen.
Verwijzen
Als advisering door de JGZ niet haalbaar en/of niet effectief is, dan is verwijzing naar een (kinder)diëtist voor een dieetadvies op maat of naar een pedagoog/gedragstherapeut voor hulp bij opvoedingsproblemen raadzaam.
4.4 Follow-up
De JGZ blijft de groei ook na verwijzing volgen. Met de behandelend kinderarts of huisarts kunnen afspraken worden gemaakt over de follow-up van de groei. Follow-up kan, ook als het kind in de eerste of tweede lijn onder behandeling is, door de JGZ worden gedaan. Duidelijke afspraken over het aantal en de frequentie van de controle(s) en wanneer het kind terug verwezen moet worden zijn dan nodig. De advisering en begeleiding van de jeugdige met ondergewicht en zijn/haar ouders blijft de verantwoordelijkheid van de hoofdbehandelaar, de JGZ vraagt wel tijdens reguliere contacten of het lukt de adviezen op te volgen.
Aanbevelingen
4.5 Informatie voor ouders en jeugdigen/lotgenotencontact
De JGZ-professional kan ouders en jeugdigen voor algemene informatie over gezonde voeding en een gezond gewicht wijzen op de informatie op de website van het Voedingscentrum. Op Mijn Voedingscentrum kunnen zij ook de Eetmeter invullen om inzicht te krijgen in wat de jeugdige eet en, indien gewenst, meenemen bij het bezoek aan de JGZ. De website Groeigids.nl geeft informatie voor ouders over opvoeden, opgroeien en gezondheid. Met de iGrow app en de GroeiGids app (via resp. App store en Google Play) kunnen ouders zelf bijhouden hoe hun kind groeit. In Bijlage 7 van deze richtlijn wordt deze informatie voor ouders van jeugdigen met ondergewicht gebundeld. Nee-Eten! is een vereniging voor ouders van kinderen met chronische voedselweigering en sondevoeding, zie de website Nee-eten.nl.
5 Totstandkoming
5.1 Werkgroepleden
Tabel 7.1 Leden van de werkgroep
| Naam | Functie | Organisatie |
| Koen Joosten (voorzitter) | Kinderarts-intensivist | Stuurgroep Ondervoeding/ NVK/ Erasmus MC |
| Irene Grondel | Jeugdarts 0-4 jarigen | AJN |
| Gea Vrieze | Jeugdarts 0-18 jarigen | AJN/ GGD Hart voor Brabant |
| Jeroen de Wilde | Jeugdarts 4-19 jarigen en onderzoeker | AJN/ GGD Haaglanden |
| Annemarie van Elburg | Kinder- en jeugdpsychiater | GGZ-kinderpsychiater |
| Annemarie Schalkwijk | Huisarts | NHG |
| Brenda Glas | Voedingsdeskundige/ Kinderdiëtist | NVD |
| Mathilde Buijs | Doktersassistente 0-19 jarigen | NVDA |
| Annemiek van den Berg | Lactatiekundige/ jeugdverpleegkundige Icare JGZ | NVL |
| Dieuwertje Stompedissel | Logopediste | NVLF |
| Tom van Bolderen | Stafmedewerker | SeysCentra |
| Daniel Seys | Orthopedagoog | SeysCentra |
| Petra Luttekes | Ouder | Ouders & Onderwijs |
| Hester Rippen | Directeur | St. Kind en Ziekenhuis |
| Jeannette Ruesink | Verpleegkundig specialist 0-4 jarigen | V&VN |
| Lia Denekamp | Jeugd en stafverpleegkundige 0-4 jarigen | V&VN |
Tabel 7.2 Klankbordgroep en meelezers
| Naam | Functie | Organisatie |
| Jeanne-Marie Hament | Jeugdarts | AJN |
| Marie-Jose Kortenhorst | Jeugdarts | AJN |
| Annemarie Roodenburg | Adviseur JOGG-aanpak | Jongeren op Gezond Gewicht (JOGG) |
| Elisa van der Molen | Kinderdiëtist | NVD |
| Dorinde Grouwstra | Lactatiekundige | NVL |
| Fleur Sickinghe-Ledeboer | Preverbaal logopedist | NVLF |
| Joke van Wieringen | Programmamanager Jeugd | Pharos Expertisecentrum gezondheidsverschillen |
| Annemieke Goudkuil | Verpleegkundig specialist | V&VN |
| Anette Stafleu | Senior voedingskundige | Voedingscentrum |
| Annet Cornelisse | Jeugdverpleegkundige 0-12 en stafverpleegkundige | Persoonlijke titel |
| Eline Snel-Lissenberg | Jeugdarts | Persoonlijke titel |
| Irene Hoogendam | Jeugdarts | Persoonlijke titel |
| Irene Hoogendam | Jeugdarts | Persoonlijke titel |
| Petra van der Velden-Sloos | Jeugdarts in opleiding | Persoonlijke titel |
5.2 Procesbeschrijving
Voor de start van het project is een werkgroep samengesteld, deze werkgroep is bij alle fasen van de ontwikkeling van de richtlijn intensief betrokken geweest. Bij de formatie van de werkgroep is gelet op een goede balans tussen wetenschappers, inhoudelijke experts en uitvoerende JGZ professionals. Zie voor de leden van de werkgroep subsectie Werkgroepleden Tabel 7.1. Met de werkgroep leden zijn afspraken gemaakt over taken en rollen in het project.
Tijdens de eerste werkgroep vergadering (januari 2017) zijn de uitgangsvragen besproken en zo nodig nader gespecificeerd en er werd besloten op welke wijze de uitgangsvragen het beste uitgewerkt kunnen worden (evidence-based, practice-based of gemengd evidence-based/practice-based). Voor alle uitgangsvragen werd gekozen voor een gemengd evidence-based/practice-based uitwerking. Hierna is een systematisch literatuuronderzoek verricht op de uitgangsvragen (zie sectie Verantwoording).
TNO heeft de literatuur bestudeerd en samengevat. De teksten waren voor de werkgroep leden inzichtelijk en te bewerken op Google Drive. De eerste conceptversie van de richtlijn is besproken tijdens de werkgroep vergadering in september 2017. De commentaren zijn verwerkt tot conceptversie 2 en in december 2017 opnieuw beoordeeld door de werkgroep. In december 2017 is in samenwerking met het NCJ het BDS protocol opgesteld. Tevens is een klankbordgroep samengesteld. Zie subsectie Werkgroepleden Tabel 7.2 voor de deelnemers aan de klankbordgroep en de meelezers. De klankbordgroep is verantwoordelijk voor het becommentariëren en aanvullen van concepttekst vanuit ieders eigen ervaring en expertise. Het tweede concept van de richtlijn is op 22 januari 2018 ook voorgelegd aan de RAC van het NCJ en ZonMw. Naar aanleiding van de feedback op deze conceptversie is in februari 2018 een derde conceptversie opgesteld. Hierna is gestart met een praktijktest. De conceptrichtlijn is in deze periode ook verspreid voor de landelijke commentaarronde (juni t/m september 2018). De feedback die werd verzameld tijdens de praktijktest en landelijke commentaarronde werd gebruikt om de richtlijn bij te stellen.
Na het verwerken van de resultaten van de praktijktest en de landelijke commentaarronde is de richtlijn op 19 november 2018 opnieuw voorgelegd aan de RAC van het NCJ en ZonMw. Ook werden conceptindicatoren ontwikkeld. Het BDS protocol werd aangepast en voorgelegd aan de BDS redactieraad van het NCJ. Ook werd de richtlijn, naar aanleiding van de feedback van de RAC van het NCJ, aangepast. Een herziene conceptversie werd opgesteld en voorgelegd aan de RAC van het NCJ en ZonMw ter autorisatie.
5.3 Cliëntenparticipatie
De cliëntenparticipatie bij de ontwikkeling van de JGZ-richtlijn is vormgegeven door deelname van een ouder namens oudervereniging Ouders & Onderwijs aan alle werkgroep vergaderingen. Tevens werd informatie ingewonnen bij ouders van jeugdigen tot 12 jaar en bij jeugdigen zelf.
6 Verantwoording
6.1 Wetenschappelijke onderbouwing
Als eerste stap bij de ontwikkeling van de richtlijn werd gestart met een systematisch literatuuronderzoek. Gevonden artikelen werden door twee medewerkers van TNO beoordeeld op relevantie. Bij verschil van mening tussen de twee beoordelaars werd in onderling overleg consensus bereikt. Relevante artikelen werden gewaardeerd aan de hand van drie aspecten, namelijk methodologische kwaliteit, toepasbaarheid in de praktijk en toepasbaarheid binnen de Nederlandse gezondheidszorg.
Beoordelen van de kracht van het wetenschappelijk bewijs
Na selectie van de meest relevante literatuur werden de artikelen volgens de GRADE-systematiek beoordeeld op methodologische kwaliteit van het onderzoek en gegradeerd naar mate van bewijs (hoog, laag, zeer laag), waarbij afwaardering nodig kan zijn vanwege een hoog risico op vertekening, inconsistentie, ‘indirectheid’ of onnauwkeurigheid. Opwaardering vindt plaats bij een groot effect, een dosis-respons relatie en als alle plausibele ‘confounding’ een effect zou kunnen reduceren of een tegenovergesteld effect zou kunnen produceren. De conclusies in deze richtlijn zijn vervolgens getrokken op basis van alle relevante studies samen (‘body of evidence’), waarbij volgens de GRADE-systematiek de minst krachtige studie het bewijsniveau bepaald.
GRADE-methode
GRADE is een methode die voor interventievragen per uitkomstmaat een gradering aan de kwaliteit van bewijs toekent op basis van de mate van vertrouwen in de schatting van de effectgrootte (Guyatt, 2008). Een belangrijk verschil tussen GRADE en andere beoordelingssystemen (bijvoorbeeld het niveau I-IV systeem of A1-D systeem) is dat GRADE niet alleen kijkt naar het studie-design maar ook andere factoren overweegt die de kwaliteit van bewijs bepalen. Voor vragen over risicofactoren, waarde van signaleringsinstrumenten, etiologie of prognose kan GRADE (nog) niet gebruikt worden. Omdat dit in preventieve richtlijnen de meeste vragen zich op dat laatste terrein bevinden kan de GRADE-methode meestal niet als zodanig toegepast worden, wel wordt de GRADE-systematiek gehanteerd.
Indeling van de kwaliteit van bewijs of mate van zekerheid ten aanzien van de effectgrootte voor een uitkomstmaat volgens GRADE:
| Mate van zekerheid | Omschrijving |
| Groot | Het werkelijke effect ligt dicht in de buurt van de schatting van het effect. |
| Matig | Het werkelijke effect ligt waarschijnlijk dicht bij de schatting van het effect, maar er is een mogelijkheid dat het hier substantieel van afwijkt. |
| Laag | Het werkelijke effect kan substantieel verschillend zijn van de schatting van het effect. |
| Zeer laag | Het werkelijke effect wijkt waarschijnlijk substantieel af van de schatting van het effect. |
De kwaliteit van bewijs of mate van zekerheid ten aanzien van de effectgrootte wordt bepaald op basis van de volgende criteria:
| Tye Bewijs | RCT start in de categorie ‘hoog’. Observationele studie start in de categorie ‘laag’. Alle overige studietypen starten in de categorie ‘zeer laag’. |
|
| Afwaarderen | ‘Risk of bias’ | −1 Ernstig −2 Zeer ernstig |
| Inconsistentie | −1 Ernstig −2 Zeer ernstig |
|
| Indirect bewijs | −1 Ernstig −2 Zeer ernstig |
|
| Onnauwkeurigheid | −1 Ernstig −2 Zeer ernstig |
|
| Publicatiebias | −1 Ernstig −2 Zeer ernstig |
|
| Opwaarderen | Groot effect | +1 Groot +2 Zeer groot |
| Dosis-respons relatie | +1 Bewijs voor gradiënt | |
| Alle plausibele confounding | +1 zou een effect kunnen reduceren +1 zou een tegengesteld effect kunnen suggereren terwijl de resultaten geen effect laten zien |
|
Formuleren van aanbevelingen
De aanbevelingen in deze richtlijn geven antwoord op de uitgangsvragen en zijn zoveel mogelijk gebaseerd op wetenschappelijk bewijs. Voor het formuleren van aanbevelingen zijn naast de kracht van het wetenschappelijk bewijs andere aspecten van belang, waaronder de ervaring van de leden van de werkgroep en klankbordgroep, voorkeuren van jongeren en ouders, kosten, beschikbaarheid, randvoorwaarden of organisatorische aspecten. Dergelijke afwegingen worden opgenomen in de paragraaf ‘overige overwegingen’. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Een lage bewijskracht van de conclusies in het systematische literatuuronderzoek sluit een sterke aanbeveling daarom niet uit, en bij een hoge bewijskracht zijn ook zwakke aanbevelingen mogelijk.
Ter informatie werden ook buitenlandse richtlijnen aangaande ondergewicht geraadpleegd. Hiervoor is gezocht in de databases van de US National Guideline Clearinghouse (www.guideline.gov) en het Guidelines International Network (www.g-i-n.net). De uiteindelijk geformuleerde aanbeveling is het resultaat van het beschikbare bewijs in combinatie met deze overige overwegingen.
Tijdens de richtlijnontwikkeling is rekening gehouden met de implementatie van de richtlijn en de daadwerkelijke uitvoerbaarheid van de aanbevelingen. Daarbij is expliciet gelet op factoren die de invoering van de richtlijn in de praktijk kunnen bevorderen of belemmeren.
6.2 Literatuur zoekstrategie
Om op een gestructureerde manier bewijs te verzamelen zijn de uitgangsvragen waarvoor bewijs uit de literatuur moet worden verzameld omgevormd tot PICO uitgangsvragen. Hierbij wordt achtereenvolgens het volgende expliciet gemaakt: P = problem, I = intervention, C = comparison, O = outcome. De volgende PICO-uitgangsvragen zijn gehanteerd als basis voor het literatuuronderzoek:
PICO 1: Instrumenten
P: kinderen uit algemene populatie met Westerse achtergrond van 0-18 jaar (child, child preschool, infant, adolescent, newborn, toddler)
I: (signalerings-)instrumenten (BMI (body mass index), bioeletrical impedance analysis, MUAC (mid-upper arm circumference), waist circumference, weight-for-height, weight-for-age, waist-hip-ratio, waist-to-height ratio, skin folds, length/height-for-age, growth chart, growth diagram, growth standard, STRONGkids)
C: –
O: afwijkend gewicht /ondervoeding /vetvrije massa /vetpercentage /vetverdeling /quality of life (weight loss, underweight, thinness, undernutrition, malnutrition, stunting, wasting, fat free mass, (body) fat percentage, (body) fat distribution)
PICO 2: Alarmsignalen
P: kinderen uit algemene populatie met Westerse achtergrond van 0-18 jaar child, child preschool, infant, adolescent, newborn, toddler)
I: stilstaande lengtegroei (stunting/delayed growth), stilstaande ontwikkeling (delayed (psychomotoric) development), hartfrequentie (low pulse), temperatuur (low body temperature), hypotensie (hypotension), terminale ondervoeding en/of uitputting/spierzwakte (muscle weakness), hypoglycemie (hypoglycemia)
C: –
O: afwijkend gewicht /ondervoeding /vetvrije massa /vetpercentage /vetverdeling /quality of life (weight loss, underweight, thinness, undernutrition, malnutrition, stunting, wasting, fat free mass, (body) fat percentage, (body) fat distribution)
PICO 3: Advisering
P: kinderen uit algemene populatie met Westerse achtergrond van 0-18 jaar (child, child preschool, infant, adolescent, newborn, toddler)
I: prevention and (intervention or advice)
C: –
O: afwijkend gewicht /ondervoeding /vetvrije massa /vetpercentage /vetverdeling /quality of life
(weight loss, underweight, thinness, undernutrition, malnutrition, stunting, wasting, fat free mass, (body) fat percentage, (body) fat distribution)
Op basis van de PICO’s werden systematische zoekacties in relevante database zoals de Cochrane Library, Pubmed, Psycinfo en Scopus uitgevoerd (Tabel 7.1). Bij elke uitgangsvraag hoort een aparte zoekstrategie. Deze zijn kort beschreven per uitgangsvraag. Naast de literatuur uit de systematische zoekacties zijn er bij een aantal vragen ook publicaties meegenomen uit de archieven van de werkgroep leden, mits deze publicaties aan de inclusiecriteria voldeden.
Tabel 7.1 Gehanteerde zoekstrategiën en uitkomsten
| Onderwerp | Gehanteerde zoekstrategieën | Aantal artikelen | Geselecteerd |
| Instrumenten | (Child[MeSH Terms]) OR child, preschool[MeSH Terms]) OR Infant[MeSH Terms]) OR adolescent[MeSH Terms]) OR Newborn[Ti/Ab]) OR toddler[Ti/Ab]) OR Infant*[Ti/Ab]) OR child*[Ti/Ab]) OR adolescent*[Ti/Ab]) OR infant, newborn[MeSH Terms] OR youth*[Ti/Ab] OR Teenager*[Ti/Ab]) AND body mass index[MeSH Terms] OR “bioelectrical impedance analysis”[Ti/Ab] OR MUAC[Ti/Ab] OR “mid-upper arm circumference”[Ti/Ab] OR “waist circumference”[Ti/Ab] OR “weight-for-height”[Ti/Ab] OR “weight for height”[Ti/Ab] OR “weight-for-age”[Ti/Ab] OR “weight for age”[Ti/Ab] OR “waist-hip-ratio”[Ti/Ab] OR “waist hip ratio”[Ti/Ab] OR waist-hip ratio[MeSH Terms] OR waist-height ratio[MeSH Terms] OR “waist-to-height-ratio”[Ti/Ab] OR “waist to height ratio”[Ti/Ab] OR “skin fold*”[Ti/Ab] OR “length-for-age”[Ti/Ab] OR “length for age”[Ti/Ab]) OR “height-for-age”[Ti/Ab] OR “height for age”[Ti/Ab] OR “growth chart*”[Ti/Ab] OR “growth diagram*”[Ti/Ab] OR “growth standard*”[Ti/Ab] OR Strongkid*[Ti/Ab]) OR BMI[Ti/Ab] AND thinness[MeSH Terms] OR malnutrition[MeSH Terms] OR body fat distribution[MeSH Terms] OR “body fat distribution”[Ti/Ab] OR malnutrition[Ti/Ab] OR thinness[Ti/Ab] OR “weight loss”[Ti/Ab] OR underweight[Ti/Ab] OR undernutrition[Ti/Ab] OR stunting[Ti/Ab] OR wasting[Ti/Ab] OR “fat free mass”[Ti/Ab] OR “body fat percentage*”[Ti/Ab] OR “fat percentage*”[Ti/Ab] OR “fat distribution”[Ti/Ab] OR undernourishment[Ti/Ab] Filters activated: Publication date from 2007/01/01 to 2017/12/31, English, Dutch, Humans. Review; Meta-Analysis, Systematic Reviews |
440 (103 uit Cochrane, 337 uit de andere databases | 29 artikelen |
| Alarmsignalen | Child[MeSH Terms]) OR child, preschool[MeSH Terms]) OR Infant[MeSH Terms]) OR adolescent[MeSH Terms]) OR Newborn[Ti/Ab]) OR toddler[Ti/Ab]) OR Infant*[Ti/Ab]) OR child*[Ti/Ab]) OR adolescent*[Ti/Ab]) OR infant, newborn[MeSH Terms] OR youth*[Ti/Ab] OR Teenager*[Ti/Ab] AND hypotension[MeSH Terms] OR hypoglycemia[MeSH Terms] OR muscle weakness[MeSH Terms] OR hypotension[Ti/Ab] OR hypotensie[Ti/Ab] OR hypoglycemie[Ti/Ab] OR hypoglycemia[Ti/Ab] OR “muscle weakness*”[Ti/Ab] OR “stunting growth”[Ti/Ab] OR “delayed growth”[Ti/Ab] OR “low pulse”[Ti/Ab] OR “low body temperature”[Ti/Ab] OR “psychomotoric development”[Ti/Ab] OR development[Ti/Ab] AND thinness[MeSH Terms] OR malnutrition[MeSH Terms] OR body fat distribution[MeSH Terms] OR “body fat distribution”[Ti/Ab] OR malnutrition[Ti/Ab] OR thinness[Ti/Ab] OR “weight loss”[Ti/Ab] OR underweight[Ti/Ab] OR undernutrition[Ti/Ab] OR stunting[Ti/Ab] OR wasting[Ti/Ab] OR “fat free mass”[Ti/Ab] OR “body fat percentage*”[Ti/Ab] OR “fat percentage*”[Ti/Ab] OR “fat distribution”[Ti/Ab] OR undernourishment[Ti/Ab] Filters activated: Publication date from 2007/01/01 to 2017/12/31, English, Dutch, Humans. Review; Meta-Analysis, Systematic Reviews |
184 artikelen uit Cochrane 660 uit andere databases |
18 artikelen |
| Advisering | Child[MeSH Terms]) OR child, preschool[MeSH Terms]) OR Infant[MeSH Terms]) OR adolescent[MeSH Terms]) OR Newborn[Ti/Ab]) OR toddler[Ti/Ab]) OR Infant*[Ti/Ab]) OR child*[Ti/Ab]) OR adolescent*[Ti/Ab]) OR infant, newborn[MeSH Terms] OR youth*[Ti/Ab] OR Teenager*[Ti/Ab] AND intervention[Ti/Ab] OR advice[Ti/Ab] AND prevention [Ti/Ab] AND thinness[MeSH Terms] OR malnutrition[MeSH Terms] OR body fat distribution[MeSH Terms] OR “body fat distribution”[Ti/Ab] OR malnutrition[Ti/Ab] OR thinness[Ti/Ab] OR “weight loss”[Ti/Ab] OR underweight[Ti/Ab] OR undernutrition[Ti/Ab] OR stunting[Ti/Ab] OR wasting[Ti/Ab] OR “fat free mass”[Ti/Ab] OR “body fat percentage*”[Ti/Ab] OR “fat percentage*”[Ti/Ab] OR “fat distribution”[Ti/Ab] OR undernourishment[Ti/Ab] Filters activated: Publication date from 2007/01/01 to 2017/12/31, English, Dutch, Humans. Review; Meta-Analysis, Systematic Reviews |
55 artikelen uit Cochrane 193 gewone artikelen 64 reviews |
0 artikelen |
6.3 Overige overwegingen
Er is slechts beperkt relevant bewijs gevonden om de inhoud van de richtlijn op te baseren. Bij de ontwikkeling is daarom vooral gezocht naar consensus en ervaring in de werkgroep en de klankbordgroep. De advisering bij ondergewicht is vooral gebaseerd op JGZ-richtlijn ‘Voeding en eetgedrag’.
6.4 Kennislacunes
- Epidemiologie van ondergewicht en ondervoeding in Nederland;
- Vergelijking van verwijscriteria voor de signalering van ondergewicht en ondervoeding;
- Screeningsinstrument voor de signalering van ondervoeding voor de JGZ;
- Effectiviteit van advisering en interventies bij ondergewicht.
6.5 Belangenverstrengeling
Geen gemeld.
7 Bijlagen
Bijlage 1 – Meten lengte en gewicht
Bijlage 2 – BMI afkappunten
Bijlage 3 – Checklist anamnese en lichamelijk onderzoek
Bijlage 4 – Eet- en beweegdagboek 0-2 jaar
Bijlage 5 – Eet- en beweegdagboek 2-18 jaar
Bijlage 6 – Websites
Bijlage 7 – Ouderinformatie ondergewicht bij jeugdigen
Bijlage 8 – Tips motiverende gespreksvoering
Referenties
[1] Ammaniti M, Lucarelli L, Cimino S, D'Olimpio F, Chatoor I. Feeding disorders of infancy: a longitudinal study to middle childhood. The International journal of eating disorders 2012;45(2):272-80
http://dx.doi.org/10.1002/eat.20925 https://pubmed.ncbi.nlm.nih.gov/21495054[2] Bandini LG, Anderson SE, Curtin C, Cermak S, Evans EW, Scampini R, Maslin M, Must A. Food selectivity in children with autism spectrum disorders and typically developing children. The Journal of pediatrics 2010;157(2):259-64
http://dx.doi.org/10.1016/j.jpeds.2010.02.013 https://pubmed.ncbi.nlm.nih.gov/20362301[3] Bayer O, Krüger H, von Kries R, Toschke AM. Factors associated with tracking of BMI: a meta-regression analysis on BMI tracking. Obesity (Silver Spring, Md.) 2011;19(5):1069-76
http://dx.doi.org/10.1038/oby.2010.250 https://pubmed.ncbi.nlm.nih.gov/20948517[4] Bocca-Tjeertes IFA, Kerstjens JM, Reijneveld SA, de Winter AF, Bos AF. Growth and predictors of growth restraint in moderately preterm children aged 0 to 4 years. Pediatrics 2011;128(5):e1187-94
http://dx.doi.org/10.1542/peds.2010-3781 https://pubmed.ncbi.nlm.nih.gov/21987699[5] Bryant-Waugh R, Markham L, Kreipe RE, Walsh BT. Feeding and eating disorders in childhood. The International journal of eating disorders 2010;43(2):98-111
http://dx.doi.org/10.1002/eat.20795 https://pubmed.ncbi.nlm.nih.gov/20063374[6] Dubois L, Ohm Kyvik K, Girard M, Tatone-Tokuda F, Pérusse D, Hjelmborg J, Skytthe A, Rasmussen F, Wright MJ, Lichtenstein P, Martin NG. Genetic and environmental contributions to weight, height, and BMI from birth to 19 years of age: an international study of over 12,000 twin pairs. PloS one 2012;7(2):e30153
http://dx.doi.org/10.1371/journal.pone.0030153 https://pubmed.ncbi.nlm.nih.gov/22347368[7] Dunn TM, Bratman S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eating behaviors 2016;21():11-7
http://dx.doi.org/10.1016/j.eatbeh.2015.12.006 https://pubmed.ncbi.nlm.nih.gov/26724459[8] Feldman R, Keren M, Gross-Rozval O, Tyano S. Mother-Child touch patterns in infant feeding disorders: relation to maternal, child, and environmental factors. Journal of the American Academy of Child and Adolescent Psychiatry 2004;43(9):1089-97
https://pubmed.ncbi.nlm.nih.gov/15322412[9] Herwig JE, Wirtz M, Bengel J. Depression, partnership, social support, and parenting: interaction of maternal factors with behavioral problems of the child. Journal of affective disorders 2004;80(2-3):199-208
https://pubmed.ncbi.nlm.nih.gov/15207933[10] Hulst JM, Joosten KFM. Nutrition Screening: Coding after Discharge Underestimates the Prevalence of Undernutrition. Journal of the Academy of Nutrition and Dietetics 2018;118(1):33-36
http://dx.doi.org/10.1016/j.jand.2017.05.019 https://pubmed.ncbi.nlm.nih.gov/28688884[11] Jansen PW, Roza SJ, Jaddoe VW, Mackenbach JD, Raat H, Hofman A, Verhulst FC, Tiemeier H. Children's eating behavior, feeding practices of parents and weight problems in early childhood: results from the population-based Generation R Study. The international journal of behavioral nutrition and physical activity 2012;9():130
http://dx.doi.org/10.1186/1479-5868-9-130 https://pubmed.ncbi.nlm.nih.gov/23110748[12] Johnson JG, Cohen P, Kasen S, Brook JS. Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. The American journal of psychiatry 2002;159(3):394-400
https://pubmed.ncbi.nlm.nih.gov/11870002[13] Littleton HL, Ollendick T. Negative body image and disordered eating behavior in children and adolescents: what places youth at risk and how can these problems be prevented? Clinical child and family psychology review 2003;6(1):51-66
https://pubmed.ncbi.nlm.nih.gov/12659451[14] Mader U. [Orthorexia--the addiction to nourishing oneself "healthfully"]. Deutsche medizinische Wochenschrift (1946) 2004;129(14):728
https://pubmed.ncbi.nlm.nih.gov/15104091[15] Mehta NM, Corkins MR, Lyman B, Malone A, Goday PS, Carney LN, Monczka JL, Plogsted SW, Schwenk WF, . Defining pediatric malnutrition: a paradigm shift toward etiology-related definitions. JPEN. Journal of parenteral and enteral nutrition 2013;37(4):460-81
http://dx.doi.org/10.1177/0148607113479972 https://pubmed.ncbi.nlm.nih.gov/23528324[16] O'Dea JA, Chiang H, Peralta LR. Socioeconomic patterns of overweight, obesity but not thinness persist from childhood to adolescence in a 6-year longitudinal cohort of Australian schoolchildren from 2007 to 2012. BMC public health 2014;14():222
http://dx.doi.org/10.1186/1471-2458-14-222 https://pubmed.ncbi.nlm.nih.gov/24592991[17] Pearce A, Rougeaux E, Law C. Disadvantaged children at greater relative risk of thinness (as well as obesity): a secondary data analysis of the England National Child Measurement Programme and the UK Millennium Cohort Study. International journal for equity in health 2015;14():61
http://dx.doi.org/10.1186/s12939-015-0187-6 https://pubmed.ncbi.nlm.nih.gov/26242408[18] Provost B, Crowe TK, Osbourn PL, McClain C, Skipper BJ. Mealtime behaviors of preschool children: comparison of children with autism spectrum disorder and children with typical development. Physical & occupational therapy in pediatrics 2010;30(3):220-33
http://dx.doi.org/10.3109/01942631003757669 https://pubmed.ncbi.nlm.nih.gov/20608859[19] Schönbeck Y, van Dommelen P, HiraSing RA, van Buuren S. Thinness in the era of obesity: trends in children and adolescents in The Netherlands since 1980. European journal of public health 2015;25(2):268-73
http://dx.doi.org/10.1093/eurpub/cku130 https://pubmed.ncbi.nlm.nih.gov/25125574[20] Smith S, Craig LCA, Raja EA, McNeill G, Turner SW. Prevalence and year-on-year trends in childhood thinness in a whole population study. Archives of disease in childhood 2014;99(1):58-61
http://dx.doi.org/10.1136/archdischild-2013-304423 https://pubmed.ncbi.nlm.nih.gov/24197872[21] Williams PG, Dalrymple N, Neal J. Eating habits of children with autism. Pediatric nursing 2000;26(3):259-64
https://pubmed.ncbi.nlm.nih.gov/12026389[22] Wonderlich SA, Crosby RD, Mitchell JE, Thompson KM, Redlin J, Demuth G, Smyth J, Haseltine B. Eating disturbance and sexual trauma in childhood and adulthood. The International journal of eating disorders 2001;30(4):401-12
https://pubmed.ncbi.nlm.nih.gov/11746301[23] Wright CM, Parkinson KN, Drewett RF. How does maternal and child feeding behavior relate to weight gain and failure to thrive? Data from a prospective birth cohort. Pediatrics 2006;117(4):1262-9
https://pubmed.ncbi.nlm.nih.gov/16585323[24] Wright CM, Parkinson KN, Drewett RF. The influence of maternal socioeconomic and emotional factors on infant weight gain and weight faltering (failure to thrive): data from a prospective birth cohort. Archives of disease in childhood 2006;91(4):312-7
https://pubmed.ncbi.nlm.nih.gov/16397011[25] Wright C, Birks E. Risk factors for failure to thrive: a population-based survey. Child: care, health and development 2000;26(1):5-16
https://pubmed.ncbi.nlm.nih.gov/10696514[26] Anten-Kools EJ, Wouwe JV, Oudesluys-Murphy AM, Semmekrot BA. Een professionele kijk op borstvoeding. Assen: Van Gorcum 2011
[27] Joosten K.F.M., Zwart H., Hop W.C., Hulst J.M.. Ondervoeding bij eenvijfde van kinderen opgenomen in Nederlandse ziekenhuizen. Ned Tijdschr Geneeskd. 2010;154:A1825():
[28] Joosten KFM, van Waardenberg D, Kneepkens CMF. Werkboek voeding voor zieke kinderen. Amsterdam: VU University Press 2017;ISBN:9789086597703():
http://www.stuurgroepondervoeding.nl/toolkits/werkboek-voeding-zieke-kinderen[29] Multidisciplinaire richtlijn Eetstoornissen 2006
http://www.richtlijneetstoornissen.nl[30] Oskam E., Lokven E.V., Boere-Boonekamp M.M.. Nederlands leerboek jeugdgezondheidszorg, Deel B: Inhoud (7e herz. dr.) Koninklijke Van Gorcum 2013
[31] Seys DM, Rensen JHM, Obbink MHJ. Behandelingsstrategieën bij jonge kinderen met voedings en eetproblemen. Houten (etc) Bohn, Stafleu Van Loghum 2000
[32] Van den Elzen APM, Sibbles, Drs. BJ, Nieuwenhuis, Dr. EES. Failure to thrive: van symptoom naar diagnose. Praktische pediatrie 2007;2():48
[33] American Academy of Pediatrics (2008). Recommendations for preventive pediatric health care. Pediatrics 2008;2901():
[34] Bang YK, Park MK, Ju YS, Cho KY. Clinical significance of nutritional risk screening tool for hospitalised children with acute burn injuries: a cross-sectional study. Journal of human nutrition and dietetics : the official journal of the British Dietetic Association 2018;31(3):370-378
http://dx.doi.org/10.1111/jhn.12518 https://pubmed.ncbi.nlm.nih.gov/28948659[35] Becker PJ, Nieman Carney L, Corkins MR, Monczka J, Smith E, Smith SE, Spear BA, White JV. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition). Journal of the Academy of Nutrition and Dietetics 2014;114(12):1988-2000
http://dx.doi.org/10.1016/j.jand.2014.08.026 https://pubmed.ncbi.nlm.nih.gov/25458748[36] Brener ND, Mcmanus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 2003;32(4):281-7
https://pubmed.ncbi.nlm.nih.gov/12667732[37] Chourdakis M, Hecht C, Gerasimidis K, Joosten KF, Karagiozoglou-Lampoudi T, Koetse HA, Ksiazyk J, Lazea C, Shamir R, Szajewska H, Koletzko B, Hulst JM. Malnutrition risk in hospitalized children: use of 3 screening tools in a large European population. The American journal of clinical nutrition 2016;103(5):1301-10
http://dx.doi.org/10.3945/ajcn.115.110700 https://pubmed.ncbi.nlm.nih.gov/27099244[38] Elia M, Stratton RJ. Considerations for screening tool selection and role of predictive and concurrent validity. Current opinion in clinical nutrition and metabolic care 2011;14(5):425-33
http://dx.doi.org/10.1097/MCO.0b013e328348ef51 https://pubmed.ncbi.nlm.nih.gov/21832898[39] Erkan T. Methods to evaluate the nutrition risk in hospitalized patients. Turk pediatri arsivi 2014;49(4):276-81
http://dx.doi.org/10.5152/tpa.2014.2226 https://pubmed.ncbi.nlm.nih.gov/26078678[40] Hartman C, Shamir R, Hecht C, Koletzko B. Malnutrition screening tools for hospitalized children. Current opinion in clinical nutrition and metabolic care 2012;15(3):303-9
http://dx.doi.org/10.1097/MCO.0b013e328352dcd4 https://pubmed.ncbi.nlm.nih.gov/22588189[41] Himes JH, Faricy A. Validity and reliability of self-reported stature and weight of US adolescents. American journal of human biology : the official journal of the Human Biology Council 2001;13(2):255-60
https://pubmed.ncbi.nlm.nih.gov/11460871[42] Hulst JM, Zwart H, Hop WC, Joosten KFM. Dutch national survey to test the STRONGkids nutritional risk screening tool in hospitalized children. Clinical nutrition (Edinburgh, Scotland) 2010;29(1):106-11
http://dx.doi.org/10.1016/j.clnu.2009.07.006 https://pubmed.ncbi.nlm.nih.gov/19682776[43] Huybrechts I, Himes JH, Ottevaere C, De Vriendt T, De Keyzer W, Cox B, Van Trimpont I, De Bacquer D, De Henauw S. Validity of parent-reported weight and height of preschool children measured at home or estimated without home measurement: a validation study. BMC pediatrics 2011;11():63
http://dx.doi.org/10.1186/1471-2431-11-63 https://pubmed.ncbi.nlm.nih.gov/21736757[44] Huysentruyt K, Alliet P, Muyshont L, Rossignol R, Devreker T, Bontems P, Dejonckheere J, Vandenplas Y, De Schepper J. The STRONG(kids) nutritional screening tool in hospitalized children: a validation study. Nutrition (Burbank, Los Angeles County, Calif.) 2013;29(11-12):1356-61
http://dx.doi.org/10.1016/j.nut.2013.05.008 https://pubmed.ncbi.nlm.nih.gov/24103513[45] Jensen NSO, Camargo TFB, Bergamaschi DP. Comparison of methods to measure body fat in 7-to-10-year-old children: a systematic review. Public health 2016;133():3-13
http://dx.doi.org/10.1016/j.puhe.2015.11.025 https://pubmed.ncbi.nlm.nih.gov/26774698[46] Joosten KFM, Hulst JM. Prevalence of malnutrition in pediatric hospital patients. Current opinion in pediatrics 2008;20(5):590-6
http://dx.doi.org/10.1097/MOP.0b013e32830c6ede https://pubmed.ncbi.nlm.nih.gov/18781124[47] Joosten KFM, Hulst JM. Nutritional screening tools for hospitalized children: methodological considerations. Clinical nutrition (Edinburgh, Scotland) 2014;33(1):1-5
http://dx.doi.org/10.1016/j.clnu.2013.08.002 https://pubmed.ncbi.nlm.nih.gov/24050847[48] Kyle UG, Earthman CP, Pichard C, Coss-Bu JA. Body composition during growth in children: limitations and perspectives of bioelectrical impedance analysis. European journal of clinical nutrition 2015;69(12):1298-305
http://dx.doi.org/10.1038/ejcn.2015.86 https://pubmed.ncbi.nlm.nih.gov/26039314[49] Ling R.E., Hedges V., Sullivan P.B.. Nutritional risk in hospitalised children: An assessment of two instruments e-SPEN, the European e-Journal of Clinical Nutrition and Metabolism 2011;6(3):
[50] Moeeni V, Walls T, Day AS. The STRONGkids nutritional risk screening tool can be used by paediatric nurses to identify hospitalised children at risk. Acta paediatrica (Oslo, Norway : 1992) 2014;103(12):e528-31
http://dx.doi.org/10.1111/apa.12768 https://pubmed.ncbi.nlm.nih.gov/25130603[51] Novianti D., Sembiring T., Sofyani S., Faranita T., Pratita W.. Screening for nutritional risk in hospitalized children: comparison of two instruments Paediatrica Indonesiana 2017;57(3):117
[52] de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization 2007;85(9):660-7
https://pubmed.ncbi.nlm.nih.gov/18026621[53] Peng L-T, Li R, Zhao W-H, Chen Y-H, Li X-M, Chen M-Y, Cao J, Li X-N. [Nutritional risk screening and its clinical significance in 706 children hospitalized in the surgical department]. Zhongguo dang dai er ke za zhi = Chinese journal of contemporary pediatrics 2013;15(10):880-5
https://pubmed.ncbi.nlm.nih.gov/24131842[54] Reilly HM, Martineau JK, Moran A, Kennedy H. Nutritional screening--evaluation and implementation of a simple Nutrition Risk Score. Clinical nutrition (Edinburgh, Scotland) 1995;14(5):269-73
https://pubmed.ncbi.nlm.nih.gov/16843942[55] Rinninella E, Ruggiero A, Maurizi P, Triarico S, Cintoni M, Mele MC. Clinical tools to assess nutritional risk and malnutrition in hospitalized children and adolescents. European review for medical and pharmacological sciences 2017;21(11):2690-2701
https://pubmed.ncbi.nlm.nih.gov/28678315[56] Scherdel P, Dunkel L, van Dommelen P, Goulet O, Salaün J-F, Brauner R, Heude B, Chalumeau M. Growth monitoring as an early detection tool: a systematic review. The lancet. Diabetes & endocrinology 2016;4(5):447-56
http://dx.doi.org/10.1016/S2213-8587(15)00392-7 https://pubmed.ncbi.nlm.nih.gov/26777129[57] Silva AM, Fields DA, Sardinha LB. A PRISMA-driven systematic review of predictive equations for assessing fat and fat-free mass in healthy children and adolescents using multicomponent molecular models as the reference method. Journal of obesity 2013;2013():148696
http://dx.doi.org/10.1155/2013/148696 https://pubmed.ncbi.nlm.nih.gov/23844282[58] Silveira J., Pinho J.. MON-PP157: Adaptation of an Evaluation Tool for Nutritional Risk in a Pediatric Service Clinical Nutrition 2015;34, S186():
[59] Teixeira AF, Viana KDAL. Nutritional screening in hospitalized pediatric patients: a systematic review. Jornal de pediatria 2016;92(4):343-52
http://dx.doi.org/10.1016/j.jped.2015.08.011 https://pubmed.ncbi.nlm.nih.gov/26859247[60] Vegelin AL, Brukx LJCE, Waelkens JJ, Van den Broeck J. Influence of knowledge, training and experience of observers on the reliability of anthropometric measurements in children. Annals of human biology 2003;30(1):65-79
https://pubmed.ncbi.nlm.nih.gov/12519655[61] Wells JCK, Fewtrell MS. Measuring body composition. Archives of disease in childhood 2006;91(7):612-7
https://pubmed.ncbi.nlm.nih.gov/16790722[62] White M, Lawson K, Ramsey R, Dennis N, Hutchinson Z, Soh XY, Matsuyama M, Doolan A, Todd A, Elliott A, Bell K, Littlewood R. Simple Nutrition Screening Tool for Pediatric Inpatients. JPEN. Journal of parenteral and enteral nutrition 2016;40(3):392-8
http://dx.doi.org/10.1177/0148607114544321 https://pubmed.ncbi.nlm.nih.gov/25096546[63] de Wilde JA, van Dommelen P, Middelkoop BJC. Appropriate body mass index cut-offs to determine thinness, overweight and obesity in South Asian children in the Netherlands. PloS one 2013;8(12):e82822
http://dx.doi.org/10.1371/journal.pone.0082822 https://pubmed.ncbi.nlm.nih.gov/24367559[64] de Wilde JA, van Dommelen P, van Buuren S, Middelkoop BJC. Height of South Asian children in the Netherlands aged 0-20 years: secular trends and comparisons with current Asian Indian, Dutch and WHO references. Annals of human biology 2015;42(1):38-44
http://dx.doi.org/10.3109/03014460.2014.926988 https://pubmed.ncbi.nlm.nih.gov/24963814[65] . WHO Child Growth Standards based on length/height, weight and age. Acta paediatrica (Oslo, Norway : 1992). Supplement 2006;450():76-85
https://pubmed.ncbi.nlm.nih.gov/16817681[66] Wiskin AE, Owens DR, Cornelius VR, Wootton SA, Beattie RM. Paediatric nutrition risk scores in clinical practice: children with inflammatory bowel disease. Journal of human nutrition and dietetics : the official journal of the British Dietetic Association 2012;25(4):319-22
http://dx.doi.org/10.1111/j.1365-277X.2012.01254.x https://pubmed.ncbi.nlm.nih.gov/22591201[67] Wonoputri N, Djais JTB, Rosalina I. Validity of nutritional screening tools for hospitalized children. Journal of nutrition and metabolism 2014;2014():143649
http://dx.doi.org/10.1155/2014/143649 https://pubmed.ncbi.nlm.nih.gov/25298890[68] Becker P, Carney LN, Corkins MR, Monczka J, Smith E, Smith SE, Spear BA, White JV, , . Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition). Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition 2015;30(1):147-61
http://dx.doi.org/10.1177/0884533614557642 https://pubmed.ncbi.nlm.nih.gov/25422273[69] Briggs-Gowan M.J., Carter A.S., Irwin J.R., Wachtel K., Cicchetti D.V.. Brief Infant-Toddler Social and Emotional Assessment (BITSEA) Manual, Version 2.0 2002
[70] Hendrikse WH, Reilly JJ, Weaver LT. Malnutrition in a children's hospital Clin. Nutr. 1997;16():13
[71] Hulst J, Joosten K, Zimmermann L, Hop W, van Buuren S, Büller H, Tibboel D, van Goudoever J. Malnutrition in critically ill children: from admission to 6 months after discharge. Clinical nutrition (Edinburgh, Scotland) 2004;23(2):223-32
https://pubmed.ncbi.nlm.nih.gov/15030962[72] Van Heerwaarden Y. Aansluiten bij ouders van vandaag. Samen met ouders een passende route uitstippelen voor de ondersteuning van kinderen bij het opgroeien en opvoeden. NCJ - Nederlands Centrum Jeugdgezondheid, Utrecht 2012
https://www.NCJ.nl[73] Van Heerwaarden Y, Pijpers F. De kracht van zelfregie. Samen komen tot passende hulp en ondersteuning. NCJ - Nederlands Centrum Jeugdgezondheid, Utrecht 2015
https://www.NCJ.nl[74] Goodman R. The Strengths and Difficulties Questionnaire: a research note. Journal of child psychology and psychiatry, and allied disciplines 1997;38(5):581-6
https://pubmed.ncbi.nlm.nih.gov/9255702[75] Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. The British journal of psychiatry : the journal of mental science 2000;177():534-9
https://pubmed.ncbi.nlm.nih.gov/11102329[76] NVK. Richtlijn Ondergewicht 2019
https://www.NVK.nl[77] Olsen EM. Failure to thrive: still a problem of definition. Clinical pediatrics 2006;45(1):1-6
https://pubmed.ncbi.nlm.nih.gov/16429209[78] Olsen EM, Petersen J, Skovgaard AM, Weile B, Jørgensen T, Wright CM. Failure to thrive: the prevalence and concurrence of anthropometric criteria in a general infant population. Archives of disease in childhood 2007;92(2):109-14
https://pubmed.ncbi.nlm.nih.gov/16531456[79] WHO. Management of severe malnutrition: a manual for physicians and other senior health workers. Geneva: World Health Organization 1999
[80] Schönbeck Y, Talma H, van Dommelen P, Bakker B, Buitendijk SE, Hirasing RA, van Buuren S. Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PloS one 2011;6(11):e27608
http://dx.doi.org/10.1371/journal.pone.0027608 https://pubmed.ncbi.nlm.nih.gov/22110687[81] Chatoor I, Ganiban J, Colin V, Plummer N, Harmon RJ. Attachment and feeding problems: a reexamination of nonorganic failure to thrive and attachment insecurity. Journal of the American Academy of Child and Adolescent Psychiatry 1998;37(11):1217-24
https://pubmed.ncbi.nlm.nih.gov/9808934[82] Florence MD, Asbridge M, Veugelers PJ. Diet quality and academic performance. The Journal of school health 2008;78(4):209-15; quiz 239-41
http://dx.doi.org/10.1111/j.1746-1561.2008.00288.x https://pubmed.ncbi.nlm.nih.gov/18336680[83] French SA, Stables G. Environmental interventions to promote vegetable and fruit consumption among youth in school settings. Preventive medicine 2003;37(6 Pt 1):593-610
https://pubmed.ncbi.nlm.nih.gov/14636793[84] Hofman E.. Kleine eters: peuters en kleuters met eetproblemen. Amsterdam: Boom 2006
[85] Hoyland A, Lawton CL, Dye L. Acute effects of macronutrient manipulations on cognitive test performance in healthy young adults: a systematic research review. Neuroscience and biobehavioral reviews 2008;32(1):72-85
https://pubmed.ncbi.nlm.nih.gov/17629947[86] iReasearch. Evaluatieonderzoek De Gezonde Schoolkantine 2010
[87] Perry CL, Bishop DB, Taylor GL, Davis M, Story M, Gray C, Bishop SC, Mays RAW, Lytle LA, Harnack L. A randomized school trial of environmental strategies to encourage fruit and vegetable consumption among children. Health education & behavior : the official publication of the Society for Public Health Education 2004;31(1):65-76
https://pubmed.ncbi.nlm.nih.gov/14768658[88] Taras H. Nutrition and student performance at school. The Journal of school health 2005;75(6):199-213
https://pubmed.ncbi.nlm.nih.gov/16014126[89] Van den Engel-Hoek L, van Gerven M, de Groot S, van Haaften L, van Hulst K. Eet- en drinkproblemen bij jonge kinderen (4 ed.). Assen: Van Gorcum 2011
[90] Williams KE, Field DG, Seiverling L. Food refusal in children: a review of the literature. Research in developmental disabilities 2010;31(3):625-33
http://dx.doi.org/10.1016/j.ridd.2010.01.001 https://pubmed.ncbi.nlm.nih.gov/20153948[91] de Wit J. Lichamelijke gevolgen van eetstoornissen bij kinderen. In: Messer AP, Vos I de, Wolters WHG. Eetproblemen bij kinderen en adolescenten. Baarn: Ambo 1994
[92] Argumentenfabriek. Knelpuntenanalyses jeugdgezondheidszorg. 2015
Heb je suggesties voor verbetering van deze JGZ-richtlijn?
Geef jouw feedbackLET OP: print de JGZ-richtlijn in liggende afdrukstand!
Grote tabellen zijn niet volledig zichtbaar als de JGZ-richtlijn in staande afdrukstand geprint wordt. Om kleuren in de printversie goed door te laten komen, moet bij de printerinstellingen Achtergrondillustraties aangezet worden.
Disclaimer printversie JGZ-richtlijnen
De printversie van de JGZ-richtlijn bevat de algemene tekst inclusief de aanbevelingen. De wetenschappelijke onderbouwing is terug te vinden op de website, bij de aanbevelingen onder de link “Evidence”.
